Acetaminophen Safety: How to Avoid Overdose and Protect Your Liver
 Dec, 23 2025
Dec, 23 2025
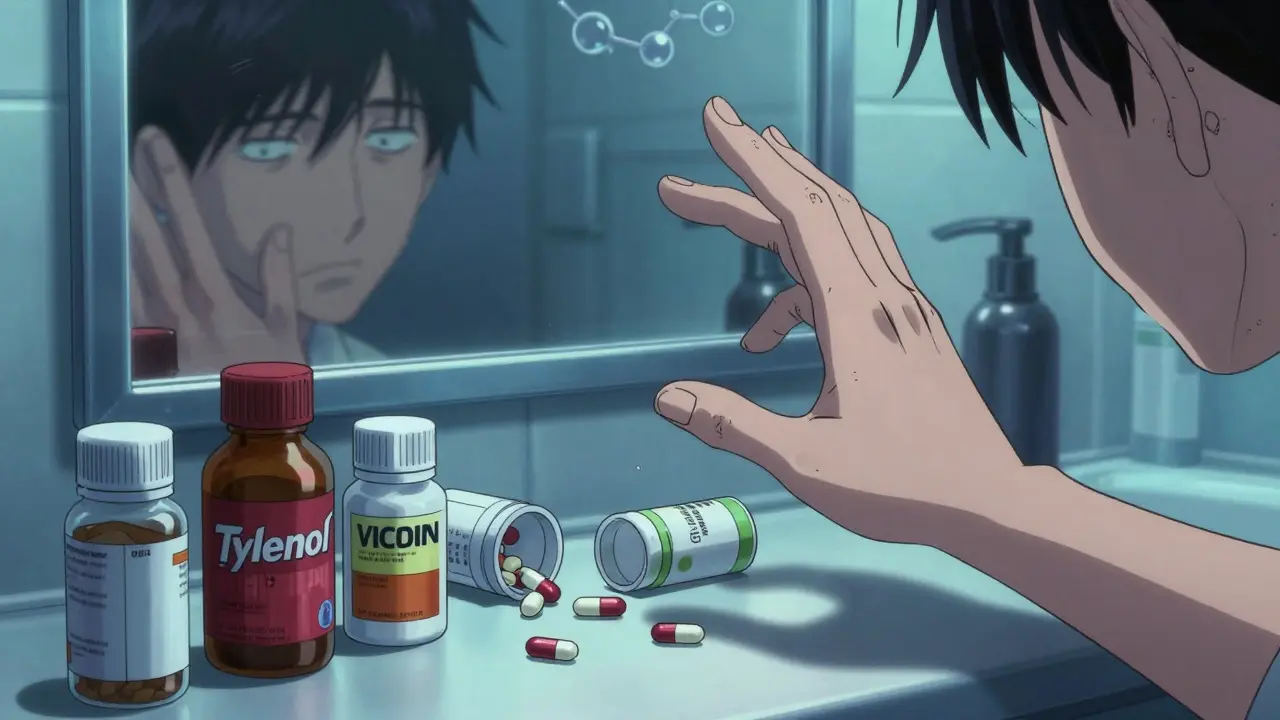
Every year, thousands of people end up in the emergency room not because they took too many pills on purpose, but because they didn’t realize how easy it is to accidentally overdose on acetaminophen. It’s in your cold medicine, your headache relief, your sleep aid, and even some prescription painkillers. You might think you’re being careful-taking just one extra tablet here, a little more when the pain won’t go away-but that small choice can push your liver into crisis.
What Acetaminophen Actually Does (and Why It’s Dangerous)
Acetaminophen, also known as paracetamol or by the brand name Tylenol, is one of the most common pain relievers in the world. It works well for headaches, fevers, muscle aches, and minor arthritis. Unlike ibuprofen or aspirin, it doesn’t irritate your stomach or increase bleeding risk. That’s why doctors often recommend it for people with ulcers, high blood pressure, or kidney issues.
But here’s the catch: the line between safe and dangerous is thin. For adults, the absolute maximum daily dose is 4,000 milligrams (4 grams). That’s eight 500mg tablets. But many experts now say even 3,000 mg per day is safer, especially if you drink alcohol or have any liver concerns. Anything over 7.5 grams in a single day can cause serious liver damage. And you don’t need to take it all at once-spreading it out over 24 to 48 hours can still be toxic.
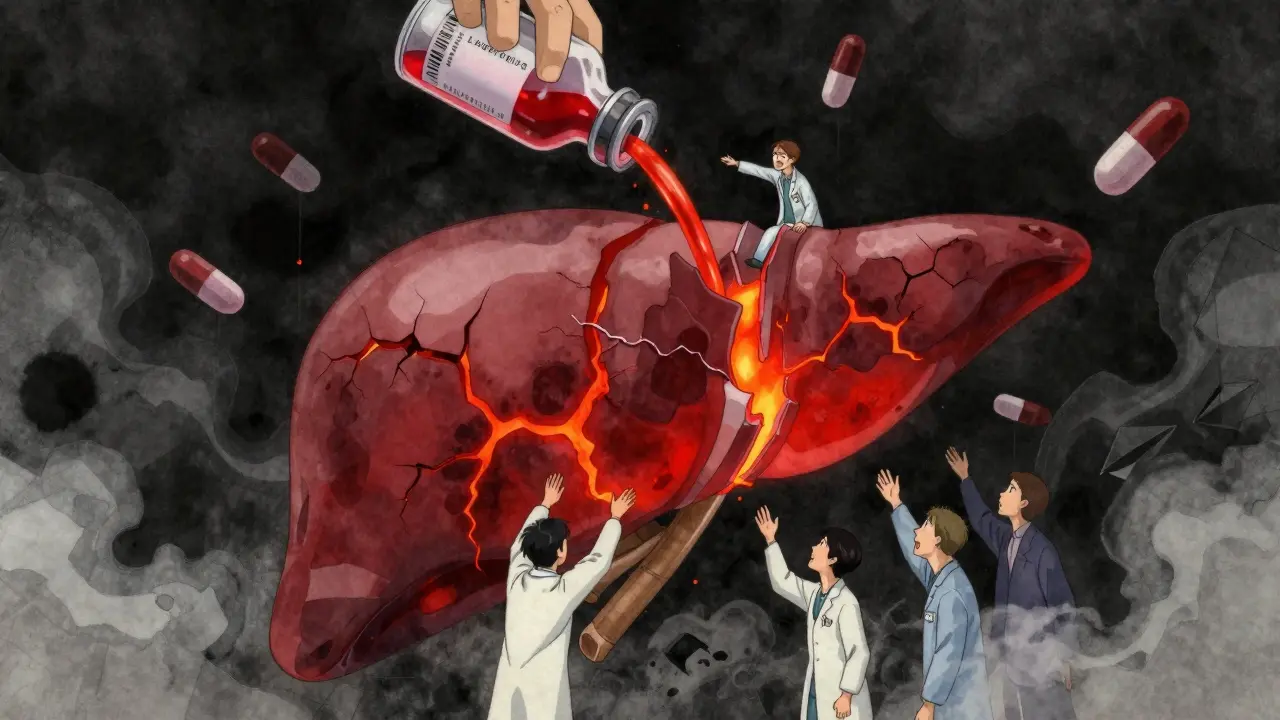
The problem isn’t the drug itself. It’s what happens inside your liver. When you take acetaminophen, your body breaks it down into harmless byproducts. But if you take too much, your liver runs out of the enzyme it needs to neutralize a toxic byproduct called NAPQI. Without enough glutathione (your body’s natural antioxidant) to mop it up, NAPQI starts killing liver cells. That’s when liver failure begins.
The Silent Progression: How Overdose Unfolds
One of the scariest things about acetaminophen overdose is how quiet it is at first. You might feel fine for 12 to 24 hours after taking too much. No vomiting. No pain. Just a little tired. That’s Stage I. But by 24 to 72 hours, your liver is already damaged-often without you knowing.
Stage II hits with sharp pain under your right ribs, nausea, and dark urine. Your blood tests will show liver enzymes like ALT and AST skyrocketing-sometimes over 10,000 IU/L (normal is under 40). By Stage III (72 to 96 hours), you’ll likely turn yellow (jaundice), feel confused, start bleeding easily, and your kidneys may fail. At this point, you’re at risk of dying without a liver transplant.
And here’s the brutal truth: if you wait too long to get help, even the antidote won’t save you. N-acetylcysteine (NAC) works best if given within 8 hours of overdose. After 16 hours, your chances of recovery drop by nearly half. Most people don’t realize they’ve taken too much until they’re already sick. That’s why prevention is everything.
Why You’re More at Risk Than You Think
You don’t have to be a drug abuser to overdose on acetaminophen. Most cases are accidental. Here’s how it happens:
- You take Tylenol for a headache, then take a cold medicine that also has acetaminophen. Two products. One dose doubled.
- You’re on Vicodin or Percocet for back pain-both contain acetaminophen-and you add extra Tylenol because the pain isn’t gone. Total dose: 6,000 mg in 12 hours.
- You’re drinking wine or beer every night and take your nightly painkiller. Alcohol makes your liver more vulnerable-even three drinks a day raises your risk.
- You use a kitchen spoon to measure liquid children’s medicine. A tablespoon instead of a teaspoon? That’s 50% more than the dose.
- You take extra-strength tablets without realizing they’re 650mg each. Four tablets = 2,600 mg. Add one cold pill? You’re already at 3,000 mg.
Studies show that 25% of accidental overdoses happen because people didn’t know two or more medications contained acetaminophen. And 23% of adults don’t even know that Tylenol is acetaminophen. The labels are small. The word “acetaminophen” is buried under “APAP” or “pain reliever.” It’s easy to miss.
How to Stay Safe: 5 Actionable Rules
You don’t need to avoid acetaminophen. You just need to use it wisely. Here’s what actually works:
- Never exceed 3,000 mg per day-even if the bottle says 4,000 mg. Lower is safer, especially if you’re over 65, have liver disease, or drink alcohol.
- Read every label. Look for “acetaminophen” or “APAP.” It’s in more than 600 products: cold medicines, sleep aids, migraine pills, prescription painkillers. Write down every medication you take and check them all.
- Avoid alcohol completely while taking acetaminophen. Even one drink a day can triple your risk of liver damage. No exceptions.
- Use the right measuring tool. For liquid forms, always use the dosing cup or syringe that comes with the bottle. Never use a kitchen spoon. A teaspoon holds 5 mL. A tablespoon holds 15 mL. That’s a 200% error.
- Keep a log. If you’re taking acetaminophen for more than a few days, write down the time and dose. Use a notes app or a small notebook. It’s the only way to track cumulative intake.
For children, dosing is based on weight: 10-15 mg per kilogram every 4-6 hours, no more than five doses in 24 hours. Never give adult tablets to kids. Always use pediatric formulations. The American Academy of Pediatrics warns that 12% of pediatric overdoses happen because parents used adult medicine by mistake.
What to Do If You Think You’ve Taken Too Much
If you realize you’ve taken too much acetaminophen-whether it’s 10 tablets, a few extra cold pills, or just one too many-you need to act fast.
- Call Poison Control immediately. In Australia, dial 13 11 26. In the U.S., call 1-800-222-1222. Don’t wait for symptoms.
- Go to the ER. Bring all your medications with you. The doctors need to know exactly what you took and when.
- Do not induce vomiting. It won’t help and could make things worse.
- Don’t assume you’re fine because you feel okay. Liver damage can be silent for hours.
People who get NAC treatment within 8 hours almost always recover fully. Those who wait beyond 16 hours face a 40% chance of liver failure. Time isn’t just important-it’s everything.

What’s Being Done to Fix This
Regulators know this is a problem. The FDA now requires all acetaminophen products to carry a “Liver Warning” on the label. But studies show only 38% of people understand what it means. In 2023, new guidelines were released to standardize how poison centers handle overdoses. There’s also a push to make “acetaminophen” appear in bold, larger text on packaging.
Some apps now scan medicine barcodes and tell you your total daily acetaminophen intake. Others alert you if you’re combining two products with the same ingredient. These tools exist-but most people don’t know about them.
Doctors are also starting to recommend lower doses for people with chronic pain, especially those with fatty liver disease or who drink regularly. The American Association for the Study of Liver Diseases now says people with existing liver conditions should cap acetaminophen at 2,000 mg per day.
Bottom Line: Respect the Dose
Acetaminophen isn’t evil. It’s a lifesaver when used right. But it’s also one of the most dangerous drugs in your medicine cabinet because it’s so easy to misjudge. You can’t feel the damage until it’s too late. There’s no warning buzzer. No stomach ache at first. Just a quiet, invisible burn inside your liver.
So check your labels. Write it down. Don’t mix it with alcohol. And if you’re ever unsure-call Poison Control. Better safe than sorry. Your liver doesn’t ask for permission before it fails. But you can ask for help before it’s too late.
Can I take acetaminophen if I drink alcohol occasionally?
It’s not recommended. Even one or two drinks a day can make your liver more sensitive to acetaminophen. The combination increases the production of the toxic metabolite NAPQI and reduces your liver’s ability to detoxify it. If you drink regularly, stick to the lowest possible dose-no more than 2,000 mg per day-and avoid daily use.
Is Tylenol safer than ibuprofen for my stomach?
Yes, acetaminophen is much gentler on the stomach than ibuprofen or aspirin, which can cause ulcers and bleeding. But that doesn’t mean it’s safer overall. While NSAIDs harm your gut, acetaminophen harms your liver. The choice depends on your health: use ibuprofen if you have liver issues, acetaminophen if you have stomach problems-but never exceed safe doses.
What’s the difference between regular and extra-strength Tylenol?
Regular Tylenol tablets contain 325 mg of acetaminophen. Extra-strength tablets contain 500 mg. That means four extra-strength tablets equal 2,000 mg-half your daily limit. If you take two extra-strength tablets every 4 hours, you’ll hit 3,000 mg in 12 hours. That’s already above the recommended safe limit for many people. Always check the label, not the brand name.
Can I take acetaminophen with prescription painkillers like Vicodin?
Only if you’re counting every milligram. Vicodin, Percocet, and similar drugs contain acetaminophen-usually 300-325 mg per tablet. If you take two Vicodin tablets, that’s already 650 mg. Add two extra-strength Tylenol tablets? You’re at 1,650 mg. Do that four times a day? You’re at 6,600 mg-dangerously over the limit. Always ask your pharmacist to calculate your total daily acetaminophen intake when you’re on multiple medications.
What are the early signs of acetaminophen overdose?
The earliest signs are subtle: nausea, vomiting, loss of appetite, sweating, and general fatigue. These can appear as early as 12 hours after overdose, but many people feel fine. Don’t wait for jaundice or severe pain. If you suspect you’ve taken too much-even if you feel okay-call Poison Control immediately. Liver damage doesn’t wait for symptoms to get worse.
Is there a blood test to check for acetaminophen overdose?
Yes. Doctors can test your blood for acetaminophen levels and liver enzymes (ALT, AST). If you’ve taken too much, these levels will rise. But the most important test is timing. A blood test within 4-24 hours after ingestion can be plotted on the Rumack-Matthew nomogram to determine if you need NAC treatment. Waiting too long makes the test less useful.
For more information on safe medication use, check with your pharmacist or visit the website of your country’s medicines regulator. Always keep your medications out of reach of children and never share prescriptions-even if you think they’ll help someone else.


Austin LeBlanc
December 24, 2025 AT 14:40Bro, I took 6 Tylenol last week for my back and drank two beers. Felt fine. Zero issues. You people are scaremongering. My liver’s tougher than your anxiety.
Also, why are we acting like acetaminophen is cyanide? It’s not. It’s a pill. Chill.
Gray Dedoiko
December 24, 2025 AT 18:09I used to be like you - until my uncle ended up in the ICU after mixing Vicodin and NyQuil. He didn’t even know NyQuil had acetaminophen. He thought he was just ‘taking something for the cold.’
Now I write down every pill I take. No shame. Better safe than sorry. Your liver doesn’t text you when it’s crying.
Paula Villete
December 25, 2025 AT 21:15Oh wow. So the FDA’s ‘Liver Warning’ is just decorative? Like those ‘may contain nuts’ labels on candy bars? I guess we’re supposed to squint and hope for the best.
Also, ‘APAP’? Who thought that was a good idea? Is this a secret code for ‘I’m gonna kill your hepatocytes’? 😏
And yes, I just used an emoticon. Sue me. I’m a sarcastic philosopher with perfect grammar and zero patience for corporate obfuscation.
Georgia Brach
December 27, 2025 AT 12:16This post is dangerously misleading. Acetaminophen is not uniquely dangerous - it’s just the most studied. Every drug has risks. Ibuprofen causes GI bleeds. Aspirin causes Reye’s syndrome. Alcohol kills more livers than acetaminophen ever has.
Blaming the drug instead of poor education is lazy. Also, 3,000 mg is arbitrary. Why not 2,500? Or 1,000? Where’s the evidence? This reads like fear-mongering dressed as public health.
Katie Taylor
December 27, 2025 AT 14:46STOP. JUST STOP. You think this is about pills? No. This is about how we treat our bodies like disposable batteries. You don’t drink and drive. Why the hell are you drinking and dosing? You don’t text and drive. Why are you taking two meds without reading the label?
This isn’t medical advice - it’s basic human responsibility. If you can’t read a bottle, maybe you shouldn’t be in charge of your own life.
Payson Mattes
December 28, 2025 AT 19:24Did you know the FDA secretly colludes with Big Pharma to keep acetaminophen on the market because it’s cheap and profitable? They don’t want you to know that NAC is a cheap antioxidant that costs pennies - but they charge $800 for it in the ER to make you dependent on the system.
Also, the liver warning? It’s only on the back of the box. They don’t want you to see it. That’s why I only take herbal supplements now. Turmeric, garlic, and moon water. Works better anyway.
Isaac Bonillo Alcaina
December 28, 2025 AT 21:24You’re all missing the point. The real danger isn’t acetaminophen - it’s the cultural normalization of self-medication. People treat medicine like candy because they’ve been conditioned to believe pain is a flaw to be erased, not a signal.
And yet, no one talks about the psychological dependency. We’re not overdosing on pills - we’re overdosing on avoidance. Your liver is just the collateral damage.
Bhargav Patel
December 29, 2025 AT 18:03In India, we have a different relationship with acetaminophen. It is commonly sold without prescription, and yet, liver toxicity from it remains relatively low. Why? Because we do not combine it with alcohol habitually, and we rely more on traditional remedies for minor ailments.
Moreover, our elders teach us to listen to the body, not the label. When the pain subsides, we stop. We do not chase comfort at the cost of function.
Perhaps the solution lies not in stricter dosing, but in cultural re-education.
Steven Mayer
December 31, 2025 AT 03:46The pharmacokinetics of acetaminophen are well-characterized: first-order metabolism via glucuronidation and sulfation, with CYP2E1-mediated oxidation to NAPQI becoming saturated above therapeutic thresholds. Glutathione depletion is the critical tipping point.
But the clinical literature consistently shows that toxicity is dose- and time-dependent, with the Rumack-Matthew nomogram providing >95% predictive accuracy for NAC efficacy when applied within 8 hours.
Yet, public messaging remains catastrophically inadequate. This isn’t a labeling problem - it’s a systems failure in pharmacovigilance.
Charles Barry
January 2, 2026 AT 00:17They don’t want you to know this, but acetaminophen is just a gateway drug. First it’s Tylenol for headaches, then it’s Percocet for ‘back pain,’ then it’s opioids because your liver’s too fried to handle anything else.
And the FDA? They’re on the payroll. The same people who approved OxyContin are the ones who let ‘APAP’ slide on every other bottle.
Wake up. This isn’t an accident. It’s a slow-motion opioid epidemic with a different name.
Rosemary O'Shea
January 2, 2026 AT 23:10Oh, how quaint. A 12-page treatise on acetaminophen, as if we’re all 18-year-olds who just discovered painkillers. Meanwhile, in the real world, people take one pill and die. Why? Because they’re not reading labels - they’re scrolling TikTok.
And you think education will fix this? Honey, the average American can’t find the ‘back’ button on their phone. You really believe they’ll read a footnote that says ‘APAP’?
Joe Jeter
January 4, 2026 AT 20:52Everyone’s acting like this is new. It’s not. I’ve been warning people since 2012. You think this is about liver damage? No. It’s about control. They want you dependent on pills so you won’t question the system.
Also, why is this post full of ‘actionable rules’? Who gave you the right to tell me how to live? I’ll take what I want, when I want. Your rules don’t apply to me.
Sidra Khan
January 6, 2026 AT 15:10So… if I take 3000mg of Tylenol and a glass of wine, I’m basically doing a liver version of Russian roulette? 🤡
Also, I just Googled ‘APAP’ and it’s just ‘acetaminophen’ backwards. Who thought that was a good idea? Someone with a PhD in chaos, I assume.
Lu Jelonek
January 7, 2026 AT 13:20As a nurse in a rural ER, I’ve seen this too many times. A grandmother takes her arthritis meds, then takes her granddaughter’s cold syrup because ‘it looks the same.’
She doesn’t speak English well. The label is tiny. The pharmacy didn’t explain it. No one asked.
This isn’t negligence - it’s systemic failure. We need multilingual labels, pharmacist counseling, and mandatory alerts in EHRs. Not just another Reddit post.
Ademola Madehin
January 8, 2026 AT 07:14Bro, I took 10 paracetamol last week and went to the club. No problem. My liver is Nigerian steel. You all scared of a little painkiller? 😂
Here in Nigeria, we just drink palm wine and take the pill - no big deal. Your bodies too soft. We built empires on less.