APOL1 Genetic Risk: Understanding Kidney Disease Disparities in African Ancestry
 Feb, 4 2026
Feb, 4 2026
Over 70% of the extra kidney disease risk in people with African ancestry comes from a single gene. This isn’t just about statistics-it’s a key to understanding why kidney disease affects some communities more severely. Let’s break down what APOL1 genetic risk is, how it works, and what it means for your health.
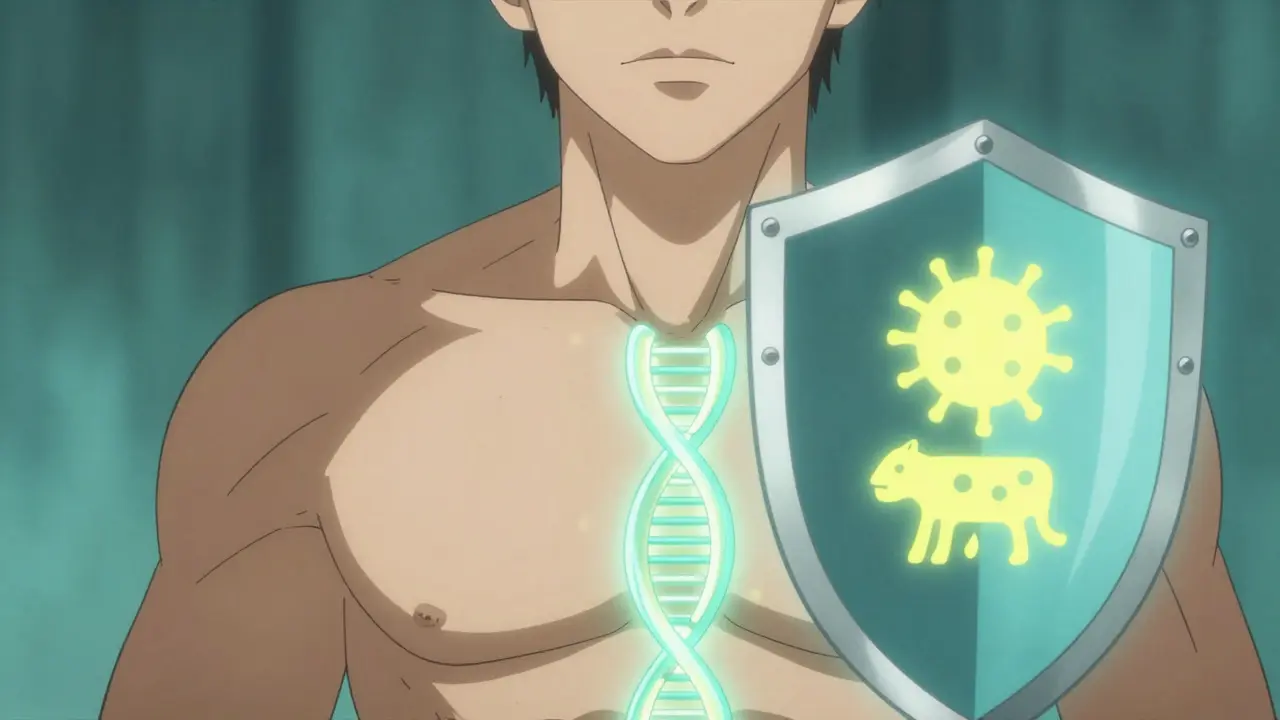
What is APOL1?
APOL1 is a gene that produces a protein involved in the immune system. Certain variants of APOL1 significantly increase the risk of kidney disease in people with recent African ancestry. This gene was discovered through studies looking at why African Americans develop kidney failure at rates three to four times higher than European Americans. The answer lies in two specific variants of APOL1: G1 and G2. These variants evolved in West Africa thousands of years ago as a defense against African sleeping sickness, a deadly parasite spread by tsetse flies. While these changes saved lives from infection, they accidentally created a hidden risk for kidney disease today.
How APOL1 Variants Work
The G1 and G2 variants of APOL1 are recessive. That means you need two copies-one from each parent-to have high-risk status. About 13% of self-identified African Americans carry these high-risk genotypes (either G1/G1, G2/G2, or G1/G2). But here’s the twist: 70% of people with these variants never develop kidney disease. This shows the risk isn’t guaranteed. Something else, like HIV infection, high blood pressure, or other environmental factors, often triggers kidney damage. For example, in people with HIV, about 49% of end-stage kidney disease cases in African ancestry populations are directly linked to APOL1 variants.
Why This Matters for Kidney Health
APOL1 variants explain most of the racial gap in kidney disease rates. African Americans face higher risks of specific kidney conditions like focal segmental glomerulosclerosis (FSGS) and HIV-associated nephropathy (HIVAN). Focal segmental glomerulosclerosis (FSGS) is a type of kidney disease where scar tissue forms in the kidney’s filtering units. APOL1 high-risk variants are a leading cause of FSGS in people of African descent. Similarly, HIV-associated nephropathy (HIVAN) is a severe kidney condition linked to HIV infection. APOL1 variants are responsible for a large portion of HIVAN cases in African ancestry populations. Without APOL1, the disparity in kidney disease rates between African Americans and European Americans would shrink dramatically. It’s a clear example of how evolution can have unintended consequences in modern environments.
Testing for APOL1 Risk
Genetic testing for APOL1 became available in 2016. Tests cost $250-$450 without insurance and are offered by labs like Invitae and Fulgent Genetics. The National Institutes of Health recommends testing for living kidney donors of African ancestry to ensure donor safety. However, many doctors still struggle to explain results clearly. A 2022 survey found 78% of nephrologists felt inadequately trained to counsel patients about APOL1. Common misunderstandings include thinking high-risk means certain kidney disease (it’s actually a 15-20% lifetime risk) or that the test is race-based (it’s about ancestry, not social race categories).
What to Do If You Have High-Risk APOL1
If you test positive, don’t panic. Most carriers stay healthy. But proactive steps matter. The American Society of Nephrology’s 2023 guidelines recommend:
- Annual urine albumin-to-creatinine ratio tests to check for early kidney damage
- Strict blood pressure control (target below 130/80 mmHg)
- Managing conditions like diabetes or HIV that act as "second hits"
- Avoiding kidney-toxic medications like NSAIDs (ibuprofen, naproxen)
Take Emani’s story as an example. She discovered her APOL1 status before kidney damage occurred. By monitoring her blood pressure and urine regularly, she preserved her kidney function for over five years. Early detection is everything.
Current Research and Future Treatments
Scientists are racing to develop therapies targeting APOL1. Vertex Pharmaceuticals’ drug VX-147 showed 37% reduction in proteinuria (a key kidney damage marker) in a 2023 trial. The NIH launched the APOL1 Observational Study in 2023, tracking 5,000 people with high-risk genotypes for 10 years to identify triggers and protective factors. Meanwhile, the Global Kidney Health Atlas found only 12% of low- and middle-income countries have access to APOL1 testing, highlighting urgent equity gaps. If successful, APOL1-targeted treatments could reduce racial disparities in kidney failure by 25-35% by 2035.
Ethical Considerations: Race vs. Ancestry
It’s critical to separate social race from genetic ancestry. APOL1 variants are tied to West African ancestry, not race as a social construct. Dr. Olugbenga Gbadegesin, a Vanderbilt University professor, warns: "Conflating race with genetic ancestry can lead to harmful stereotypes." For example, the American Medical Association’s 2022 policy discourages race-based kidney function calculations because APOL1 research shows genetic factors matter more than race categories. This distinction ensures fair treatment and avoids blaming communities for biological differences.
Frequently Asked Questions
Can APOL1 testing be done during routine checkups?
Yes, but it’s usually not part of standard blood tests. You’ll need to request it specifically, especially if you have a family history of kidney disease or are of African descent. Nephrologists or genetic counselors typically order these tests. Insurance coverage varies-some plans cover it if there’s a clear medical reason, like unexplained kidney damage.
If I have APOL1 variants, will my children inherit the risk?
Yes, APOL1 variants are inherited. Each child has a 25% chance of getting two copies (high-risk), 50% chance of one copy (low-risk carrier), and 25% chance of no copies. Genetic counseling is recommended before having children if you know you carry high-risk variants. However, remember most carriers never develop kidney disease, so this isn’t a guarantee of future illness.
Are there any lifestyle changes that can reduce APOL1-related kidney risk?
Absolutely. Controlling blood pressure is the most effective step-aim for below 130/80 mmHg. Avoid smoking, limit salt intake, and manage conditions like diabetes or obesity. Staying hydrated and avoiding NSAIDs (e.g., ibuprofen) also protects kidney function. While you can’t change your genes, these actions significantly lower the chance of "second hits" triggering kidney damage.
Why do APOL1 variants affect kidney cells but not other organs?
APOL1 proteins are most active in kidney cells called podocytes, which filter blood. The risk variants cause these proteins to form abnormal pores in cell membranes, leading to cell death. Other organs either don’t produce much APOL1 or have protective mechanisms. Research shows the kidney’s unique environment makes it especially vulnerable to these changes, explaining why kidney disease is the primary concern.
Is APOL1 testing recommended for all African Americans?
Not routinely. Testing is most useful for people with unexplained kidney disease, family history of kidney failure, or those considering kidney donation. For healthy individuals without symptoms, the benefits are unclear since most carriers never develop disease. The American Society of Nephrology advises against widespread screening until better tools exist to predict who will actually get sick.


Jennifer Aronson
February 6, 2026 AT 07:36The APOL1 gene's history is fascinating. It evolved in West Africa thousands of years ago as a defense against African sleeping sickness caused by tsetse flies. These genetic variants provided a survival advantage against the parasite. However, in modern times, the same variants now increase the risk of kidney disease. This is a classic example of evolutionary trade-offs. The key point is that 70% of the extra kidney disease risk in people with African ancestry comes from this single gene. But it's important to note that 70% of people with these high-risk genotypes never develop kidney disease. This shows the risk isn't guaranteed. Other factors like HIV, hypertension, or diabetes often act as 'second hits' that trigger kidney damage. For instance, in people with HIV, about 49% of end-stage kidney disease cases in African ancestry populations are linked to APOL1 variants. Understanding this helps separate genetic ancestry from social race. Conflating race with genetics can lead to harmful stereotypes. The American Medical Association's 2022 policy discourages race-based kidney function calculations because genetic factors matter more. It's crucial for doctors to explain APOL1 results clearly. Many patients misunderstand the risk, thinking it's certain when it's actually 15-20% lifetime risk. Proactive steps like annual urine tests and blood pressure control can help manage the risk. Overall, this research highlights how evolution shapes health in unexpected ways.
Carl Crista
February 7, 2026 AT 02:51APOL1 is a distraction Big Pharma is pushing this narrative to sell drugs They know the real cause is environmental toxins from government programs They want us to focus on genes instead of the real issues Wake up people This is a scam to profit from kidney disease treatments Check the data yourself The truth is hidden in plain sight They dont want you to know the real causes Its all about money Theyre lying to you Think for yourself Dont trust the system
Brendan Ferguson
February 7, 2026 AT 16:35The APOL1 variants are recessive so you need two copies But 70% of carriers never get kidney disease So it's about other factors like HIV or hypertension Important to manage those Also the NIH recommends testing for living kidney donors of African ancestry to ensure safety But many doctors struggle to explain results clearly A 2022 survey found 78% of nephrologists felt inadequately trained Common misunderstandings include thinking high-risk means certain kidney disease It's actually a 15-20% lifetime risk So don't panic but stay proactive
Johanna Pan
February 8, 2026 AT 03:58Brendan's right Managing blood pressure and avoiding NSAIDs is key Dont panic but stay proactive Check urine regularly Control diabetes if you have it Stay hydrated Avoid smoking Its all about reducing those second hits
Gregory Rodriguez
February 9, 2026 AT 21:50Wow APOL1 is like a double-edged sword Saved us from sleeping sickness but now we're paying the price Classic evolutionary 'oops' moment But hey at least we're getting closer to treatments Vertex Pharmaceuticals' drug VX-147 showed 37% reduction in proteinuria That's promising The NIH is tracking 5000 people for 10 years Hopefully this leads to better therapies Fingers crossed
lance black
February 11, 2026 AT 08:10Early detection and BP control save kidneys
Jenna Elliott
February 11, 2026 AT 22:18APOL1 is a distraction Pharma's hiding the real cause They profit from kidney disease The US should focus on our own health issues instead of this genetic stuff This is why we need to stop blaming race It's all about personal responsibility Stop the blame game
Sam Salameh
February 11, 2026 AT 23:43APOL1 research is crucial But we need more funding for kidney health in the US Let's support our medical community Also genetic testing should be affordable Insurance should cover it for high-risk groups This is about equity and saving lives