Brain MRI Basics: Understanding Common Neurological Findings
 Dec, 22 2025
Dec, 22 2025
When your doctor orders a brain MRI, it’s not because they’re being overly cautious-it’s because they need to see what’s happening inside your brain in a way no other test can. Unlike X-rays or CT scans, MRI doesn’t use radiation. Instead, it uses powerful magnets and radio waves to create incredibly detailed pictures of your brain’s soft tissues. This makes it the gold standard for spotting problems like strokes, tumors, multiple sclerosis, and even early signs of dementia. But what do those images actually show? And how do doctors tell the difference between normal aging and something serious?
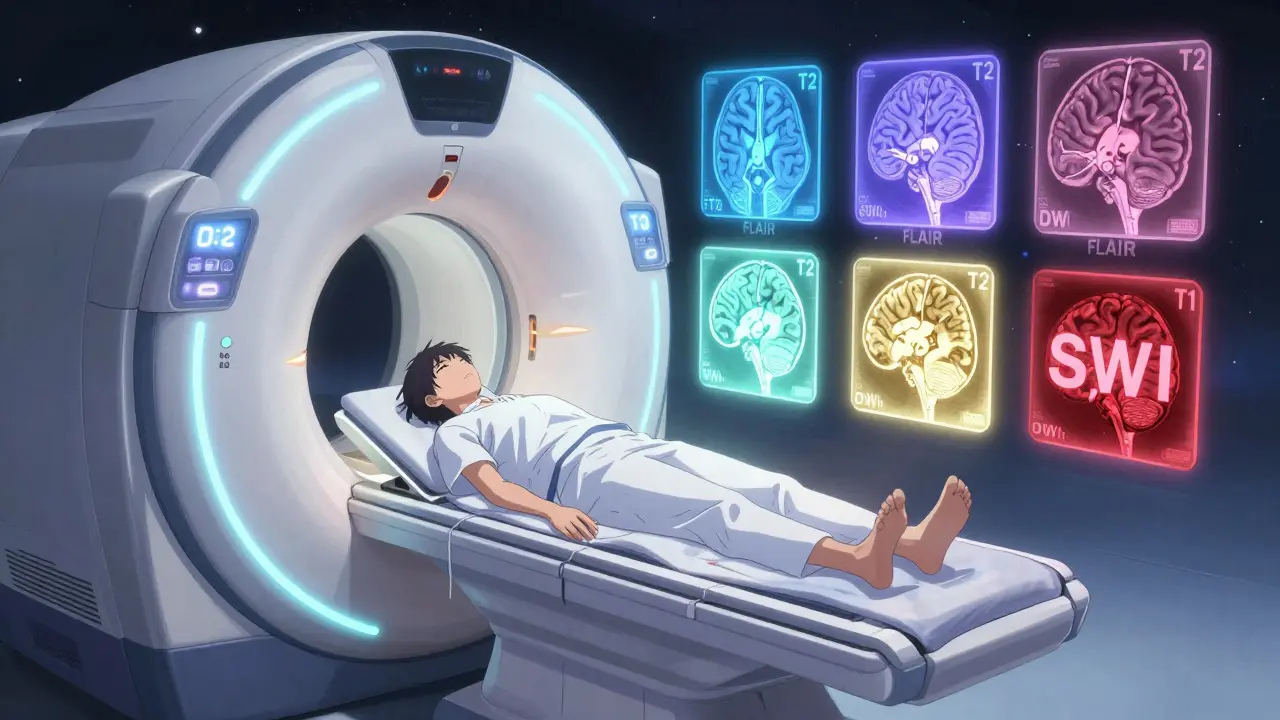
What Happens During a Brain MRI?
You lie still on a table that slides into a long, tube-shaped machine. The scan takes 30 to 45 minutes. You’ll hear loud knocking or buzzing sounds-earplugs or headphones are usually provided. No pain is involved, but staying perfectly still is critical. Even a small movement can blur the images, making it harder for the radiologist to interpret them accurately. Most brain MRIs use either a 1.5 Tesla or 3.0 Tesla magnet. The 3.0T machines give clearer pictures, especially for small structures like nerves in the inner ear or tiny blood vessels. But both are widely used. You won’t feel the magnetic field, but if you have metal implants-like a pacemaker, cochlear implant, or certain aneurysm clips-you can’t have an MRI. Safety is non-negotiable.The Five Key MRI Sequences You Need to Know
A brain MRI isn’t one picture. It’s a series of different scans, each highlighting different tissues. Think of them as different camera filters-each one reveals something new.- T1-weighted images: These show anatomy. Fat and some types of tissue look bright white. Cerebrospinal fluid (CSF)-the liquid that cushions your brain-looks dark. This is the best view to see if your brain’s structure is normal: the gray matter (outer layer), white matter (deeper tissue), and ventricles (fluid-filled spaces) should look clean and symmetrical.
- T2-weighted images: These highlight water. Anything with extra fluid-like swelling, inflammation, or a tumor-shows up bright. But here’s the catch: CSF also looks bright on T2, so it’s easy to confuse normal fluid with abnormal tissue. That’s why radiologists always check other sequences.
- FLAIR (Fluid-Attenuated Inversion Recovery): This is the most important sequence for spotting brain diseases. FLAIR turns CSF dark, but keeps abnormal fluid (like from a stroke or MS lesion) bright. That contrast makes lesions stand out clearly, especially near the ventricles. If you see bright spots around the brain’s fluid spaces, it could be multiple sclerosis, small vessel disease, or an old infection.
- Diffusion-Weighted Imaging (DWI): This is the go-to for detecting strokes that happened within the last few hours. When brain cells die from lack of oxygen, water can’t move freely. DWI picks this up immediately. If the scan shows a bright spot on DWI with a dark spot on the ADC map (a related image), it’s an acute stroke. Time matters here-this finding can change whether someone gets clot-busting drugs.
- SWI (Susceptibility-Weighted Imaging): This sequence is like a metal detector for blood. It picks up tiny amounts of iron left behind by old bleeds-even those too small to see on other scans. That’s how doctors spot microbleeds from high blood pressure, traumatic brain injury, or rare conditions like cerebral amyloid angiopathy.
Common Findings and What They Mean
Not every bright spot on an MRI means cancer or a stroke. Many findings are harmless or part of normal aging.White matter hyperintensities (WMHs)-bright spots in the brain’s white matter-are seen in 15% of people under 50 and up to 90% of those over 70. These are often linked to high blood pressure, diabetes, or just aging. They’re called “leukoaraiosis” in medical terms. Unless they’re large, widespread, or accompanied by symptoms like memory loss or trouble walking, they’re usually not treated. But if they’re growing fast, your doctor might look for underlying vascular disease.
Small lacunar infarcts are tiny strokes, often less than 5mm, caused by blocked blood vessels deep in the brain. They’re common in older adults with hypertension. You might have had one and never known it-many are silent. But if you have several, your risk of future stroke or dementia goes up.
Multiple sclerosis plaques look like bright, oval-shaped lesions on FLAIR and T2 images. They’re often found near the ventricles, in the brainstem, or along the spinal cord. What makes them different from other white matter spots? Their shape, location, and pattern. MS lesions tend to be perpendicular to the ventricles (“Dawson’s fingers”) and appear in multiple areas over time. A single lesion doesn’t mean MS-it has to fit a pattern.
Brain atrophy means the brain has shrunk. Some shrinkage is normal with age. But if the hippocampus (memory center) or cortex is noticeably smaller than expected for your age, it could point to Alzheimer’s or another neurodegenerative disease. Radiologists compare the size of brain structures to standard measurements to spot abnormal atrophy.
Incidental findings are surprises. Maybe it’s a small, harmless tumor called a meningioma, or a vestibular schwannoma (acoustic neuroma) on the nerve that connects your ear to your brain. These are often found by accident when scanning for something else. Most are slow-growing and don’t need treatment unless they cause symptoms like hearing loss or dizziness.
When MRI Is the Best Choice-and When It’s Not
MRI beats CT for almost everything except emergencies. In trauma, like after a car crash, CT is faster. It takes 5 minutes to rule out a skull fracture or bleeding. MRI takes 40 minutes. If you’re unstable, you get CT first.For headaches? MRI isn’t usually needed. The American College of Radiology says it’s “usually not appropriate” for people with typical migraines and no neurological signs. Only 1.3% of brain MRIs done for routine headaches show anything serious. But if you have new seizures, vision changes, weakness, or confusion, an MRI is essential.
For stroke, DWI MRI is the most sensitive test. It catches changes within minutes. CT might miss a stroke for hours. But if you’re in a rural hospital without MRI, CT is still life-saving.
What Doesn’t Show Up on MRI
MRI is powerful, but it’s not magic. It can’t show:- Electrical activity in the brain (that’s EEG’s job)
- Chemical imbalances like low serotonin or dopamine
- Early Alzheimer’s plaques unless you’re using a special amyloid PET scan (still mostly research)
- Psychiatric conditions like depression or anxiety
That’s why a brain MRI is only one part of the puzzle. Your symptoms, exam, and blood tests matter just as much.
How Radiologists Read an MRI
There’s a method to how experts interpret these images. They don’t just glance-they follow a routine:- Check the midline-is the brain centered, or is there a shift (which could mean a tumor or swelling)?
- Look at the ventricles-are they enlarged? That could mean atrophy or fluid buildup.
- Scan the basal ganglia and thalamus for small bright spots (old tiny strokes).
- Examine the cerebellum and brainstem-this area is hard to see on CT, but MRI catches small tumors or MS lesions here.
- Check the meninges and skull base for tumors or inflammation.
- Compare both sides-is everything symmetrical?
One common mistake new readers make? Mistaking blood vessels for lesions. Vessels appear as dark, flowing lines on T2 and FLAIR-they’re called “flow voids.” If you see them, don’t panic. They’re normal.
What Comes Next After an MRI?
If your scan is normal, and your symptoms are mild, you might just need follow-up. If something’s found, the next step depends on what it is:- Small white matter changes? Control blood pressure, manage cholesterol, exercise.
- Multiple sclerosis? Neurologist referral for blood tests and possibly spinal fluid analysis.
- Acute stroke? Emergency treatment begins immediately.
- Incidental tumor? Often monitored with repeat MRIs every 6-12 months.
Don’t rush to Google your results. A single bright spot on an MRI doesn’t equal a diagnosis. Many people have findings that never cause problems. The key is context: your symptoms, age, medical history, and the pattern of changes.
The Future of Brain MRI
New tech is making MRI even better. Artificial intelligence can now cut scan time in half without losing detail. Some hospitals are using ultra-high-field 7.0T machines to see brain layers as thin as 0.5mm-something impossible just a decade ago. Researchers are also developing quantitative MRI measures: mapping how much water is in myelin (the brain’s insulation), or how fast blood flows in tiny vessels. These could one day diagnose Alzheimer’s before memory loss starts.But for now, the 1.5T and 3.0T machines you’re likely to get are still the most reliable tools we have. They’ve saved countless lives by spotting problems too small for other tests to catch.
Is a brain MRI safe?
Yes, for most people. MRI uses no radiation. But it’s not safe if you have certain metal implants like pacemakers, cochlear implants, or some types of surgical clips. Always tell your doctor about any metal in your body before the scan. The magnetic field is extremely strong-it can pull loose metal objects into the machine at high speed. Even tattoos with iron-based ink can sometimes heat up, though this is rare.
Can I have an MRI if I’m claustrophobic?
Many people feel anxious in the narrow tube. Open MRI machines exist but offer lower image quality. Most facilities offer sedation if needed. Some newer MRI machines are wider and shorter, making them less confining. You can also ask for music, a mirror to see outside, or have a friend stay in the room (if they’re cleared for safety). Breathing slowly and focusing on something calming helps a lot.
Why do I need contrast dye for some brain MRIs?
Gadolinium-based contrast helps highlight areas where the blood-brain barrier is broken-like in tumors, infections, or active MS plaques. It makes these areas glow brighter on T1 images. Not every scan needs it. If you have kidney problems, your doctor will check your kidney function first, as rare cases of complications can occur. The contrast is generally very safe and is cleared by the kidneys within hours.
How long does it take to get MRI results?
The scan itself takes 30-45 minutes. The radiologist usually sends a report to your doctor within 24-72 hours. In urgent cases, like suspected stroke, results can be available within an hour. Don’t expect immediate results-radiologists need time to carefully compare sequences and rule out artifacts. Your doctor will discuss the findings with you in context.
Can an MRI show if I have dementia?
MRI can’t diagnose dementia directly, but it can show signs that point to it. For example, shrinkage of the hippocampus is common in Alzheimer’s. Widespread white matter damage suggests vascular dementia. In rare cases, it can spot other causes like normal pressure hydrocephalus or brain tumors that mimic dementia. But dementia diagnosis always combines MRI with memory tests, medical history, and sometimes PET scans.
Are brain MRI findings always serious?
No. Many people have small white matter spots, mild atrophy, or incidental tumors that never cause symptoms. These are often called “incidentalomas.” Finding something on an MRI doesn’t mean you have a disease-it just means you have a finding. Your doctor will look at your symptoms, age, and risk factors to decide if it matters. Overinterpreting minor findings can lead to unnecessary stress and tests.


Diana Alime
December 24, 2025 AT 09:51So basically if u have a headache and get an MRI u r basically paying $2k to find out u didnt have a brain tumor lol. My cousin got one for migraines and the doc said "its all in your head" but like... literally not in the way u think.
Georgia Brach
December 25, 2025 AT 00:09The notion that MRI is the "gold standard" for dementia is misleading. No imaging modality can diagnose neurodegenerative disease in isolation. Overreliance on structural findings leads to diagnostic inflation, misattribution of normal aging as pathology, and unnecessary patient anxiety. The clinical context is not merely supplementary-it is foundational.
Adarsh Dubey
December 26, 2025 AT 22:05Really appreciate this breakdown. I work in a rural clinic and we don't always have MRI access. Knowing what each sequence shows helps me explain to patients why we might need to refer them out-or why we don't. Especially the part about DWI for strokes. That’s life-saving info.
Bartholomew Henry Allen
December 28, 2025 AT 02:06Any country that allows non-emergency MRIs without prior military-grade clearance for metal implants is a danger to national health security. We must enforce stricter protocols. The magnetic field is not a suggestion. It is a weapon. And Americans are too soft to understand that.
Dan Gaytan
December 29, 2025 AT 03:06This is so helpful!! 🙌 I had a friend panic over white matter spots and now I can actually explain to her why it’s probably just aging + high blood pressure. So many people freak out over MRI results without context. Thanks for breaking it down so clearly!
Usha Sundar
December 30, 2025 AT 10:30FLAIR is the MVP.
Delilah Rose
December 31, 2025 AT 08:10I’ve been reading up on this since my dad’s scan showed some white matter hyperintensities, and honestly, the more I learn, the more I realize how much we don’t know. It’s terrifying to think that something so common-like these little bright spots-could be harmless or could be the first sign of something that won’t show up for years. I just wish doctors spent more time explaining what "probably benign" really means, because for families like mine, it feels anything but.
Bret Freeman
January 1, 2026 AT 22:35Let me guess-the next thing you’ll tell us is that 7T MRIs are the future and we should all be thrilled. Newsflash: the healthcare system is already broken. People are being diagnosed with "silent strokes" they never had symptoms for, then sold a $12,000 supplement regimen. This isn’t medicine. It’s fear-based revenue generation disguised as science.
niharika hardikar
January 3, 2026 AT 14:20It is imperative to underscore that the presence of Dawson’s fingers on FLAIR sequences constitutes a radiological criterion for dissemination in space per McDonald criteria. Absent clinical correlation, however, this finding remains non-diagnostic and may represent a nonspecific inflammatory response to vascular etiologies. Misinterpretation of this pattern contributes significantly to iatrogenic morbidity.
John Pearce CP
January 3, 2026 AT 21:57AI is reducing scan time. That’s fine. But when you cut corners on diagnostic rigor, you’re not advancing medicine-you’re commodifying it. The radiologist’s eye is irreplaceable. The algorithm doesn’t know your patient’s history. It doesn’t know if they’ve been depressed for a year or if their mother died of MS. Don’t let silicon replace sanity.
Katie Taylor
January 4, 2026 AT 09:50YES. This is exactly what people need to hear. Stop Googling your MRI results. You’re not a radiologist. You’re not a neurologist. You’re a person who just wants to know if they’re going to be okay. And the answer is often: yes, you are. This post is a gift.
Payson Mattes
January 4, 2026 AT 15:43Did you know the government uses MRI data to track brain patterns for mind control? The contrast dye? It’s not gadolinium-it’s a nanotech tracer that syncs with satellites. That’s why they say it’s "safe." They want you to think it’s safe. The real danger is the silent activation of neural pathways during scans. I’ve seen it happen to three people. They all started hearing whispers after their MRIs. Don’t get scanned unless you absolutely must.