Bursitis and Tendinitis: Understanding Joint Inflammation and How to Treat It
 Dec, 16 2025
Dec, 16 2025
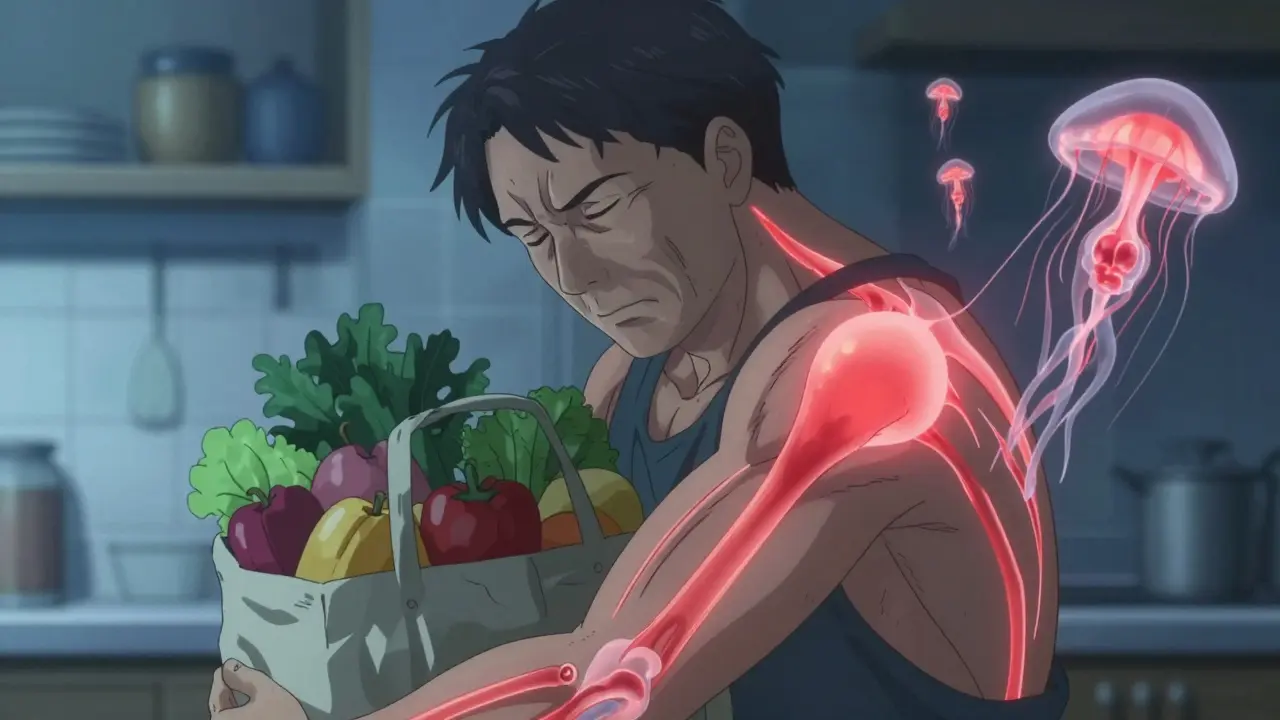
When your shoulder aches after lifting groceries, or your knee hurts when you kneel to clean the floor, it’s easy to blame aging or overuse. But what if the real culprit isn’t just wear and tear-it’s inflammation in the soft tissues around your joint? Two common conditions, bursitis and tendinitis, are behind many of these nagging pains. They’re not the same, but they often show up together-and treating them the wrong way can make things worse.
What’s the Difference Between Bursitis and Tendinitis?
Bursitis and tendinitis both cause joint pain, but they affect different parts. Think of your joints like a machine. Tendons are the strong cords that connect muscles to bones. When you move your arm or leg, your muscles pull on these tendons to make it happen. If those tendons get irritated from too much repetition-like painting ceilings, swinging a tennis racket, or typing all day-they swell up. That’s tendinitis.
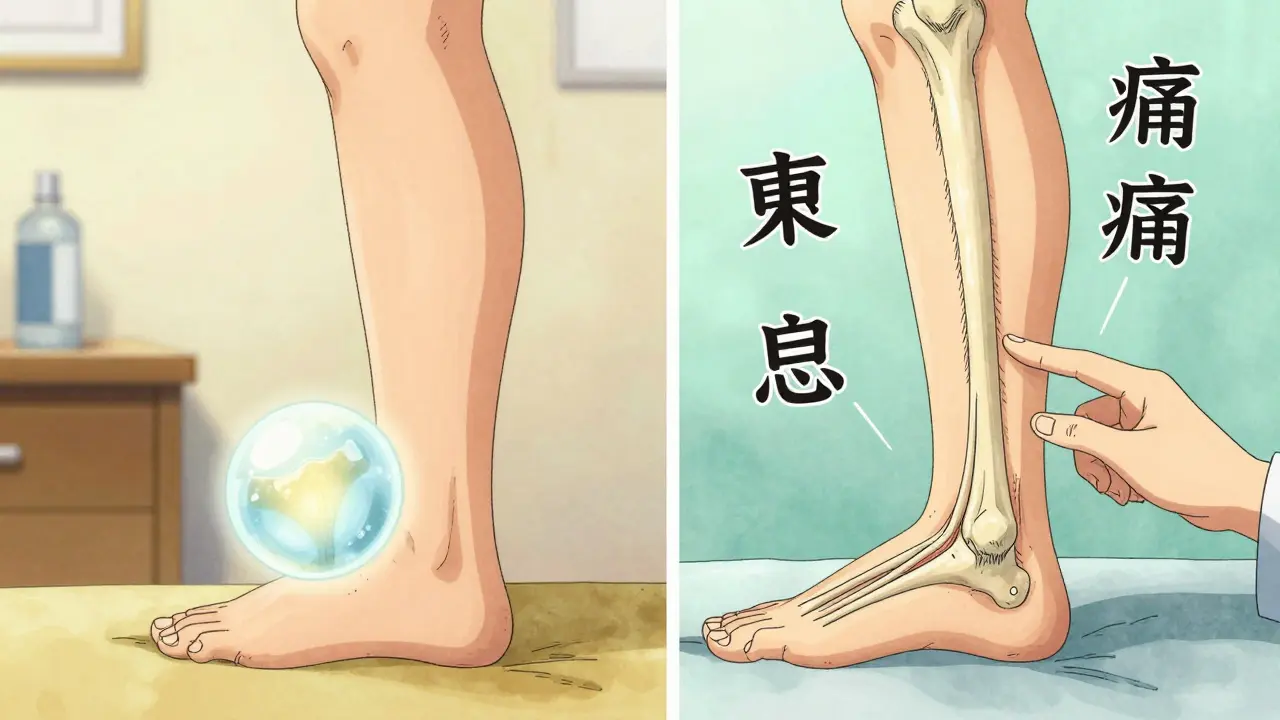
Bursae, on the other hand, are tiny fluid-filled sacs that act like cushions between bones and tendons or skin. They reduce friction so your joints glide smoothly. When those sacs get inflamed-usually from repeated pressure or a direct blow-you get bursitis. Common spots? The shoulder, elbow, hip, and knee.
Here’s how to tell them apart by feel:
- Tendinitis pain follows the path of the tendon. If your Achilles tendon is inflamed, you’ll feel it along the back of your ankle, especially when you push off your foot.
- Bursitis pain is more spread out. If your hip bursa is swollen, you’ll feel a dull ache on the outside of your hip that gets worse when you lie on that side at night.
And here’s a key detail most people miss: tendinitis often hurts more during movement, while bursitis hurts more with pressure or at rest. That’s why lying on your sore shoulder at night can wake you up-but lifting your arm might not hurt as much until you try to reach for something.
Who Gets These Conditions-and Why?
You don’t have to be an athlete to get bursitis or tendinitis. In fact, the biggest risk factor isn’t sports-it’s age. After 40, your tendons and bursae start losing their elasticity. By 50, about one in seven adults has symptoms of one or both conditions, according to the Medicare Current Beneficiary Survey.
But it’s not just aging. Repetitive motion is the real trigger. Construction workers who kneel all day? High risk for prepatellar bursitis. Musicians? Shoulder and wrist tendinitis are common. Office workers typing for hours? De Quervain’s tendinitis in the thumb can creep in.
Even your posture plays a role. Slouching at your desk puts extra strain on your shoulder tendons. Wearing worn-out shoes changes how your foot hits the ground, stressing your Achilles tendon. And if you’ve had a previous injury-even one years ago-that area is more likely to flare up again.
How Doctors Diagnose Them
Most of the time, a doctor can tell the difference just by asking you to move and pressing on the sore spot. They’ll check for:
- Localized tenderness over the tendon or bursa
- Pain that worsens with specific movements
- Swelling or warmth around the joint
But here’s the catch: imaging isn’t always helpful. A 2022 study found that 40% of people over 50 show signs of bursitis or tendinitis on an MRI-even if they have no pain at all. That means seeing inflammation on a scan doesn’t automatically mean it’s the source of your pain.
Ultrasound is more useful. It’s real-time, cheap, and picks up fluid buildup in bursae or thickening in tendons with 92% accuracy. But even ultrasound isn’t perfect. The real diagnostic tool is still the physical exam-and your description of what hurts and when.
Treatment: What Actually Works
The good news? Most cases get better without surgery. The bad news? Many people rush into the wrong treatment.
Here’s the step-by-step approach backed by clinical guidelines:
- Rest and ice for the first 7-10 days. Don’t stop moving entirely, but avoid anything that hurts. Use ice packs for 15 minutes, 3-4 times a day. A frozen water bottle rolled under your foot or along your arm works just as well as a commercial ice pack.
- NSAIDs like ibuprofen or naproxen can help reduce pain and swelling-but only for 10-14 days. Long-term use increases stomach bleeding risk, according to the Annals of Internal Medicine.
- Move gently. After the initial pain settles, start slow range-of-motion exercises. Stiffness makes recovery harder. A physical therapist can teach you how to move without re-injuring the area.
- Strengthen the right way. For tendinitis, eccentric exercises are gold standard. That means slowly lowering your heel from a step (for Achilles tendinitis) or lowering a dumbbell with control (for shoulder tendinitis). One study showed 68% of patients improved after 6 months of this method, compared to just 41% who only got cortisone shots.
- Corticosteroid injections help bursitis more than tendinitis. One 2023 study found 78% of bursitis patients felt better within four weeks after a shot. But for tendons? Only 52% improved-and the shot can weaken the tendon over time. Doctors now limit these to 2-3 per year.
And here’s the rule most people ignore: stay below 3 out of 10 pain during rehab exercises. If you feel sharp pain, you’re pushing too hard. That’s not “no pain, no gain”-that’s “more pain, more damage.”
What Doesn’t Work-and Why
Too many people try the wrong thing:
- Stretching a painful tendon can make it worse. Stretching is good for tight muscles, but not for inflamed tendons. You need strengthening, not pulling.
- Massaging the sore spot might feel good temporarily, but it can increase inflammation. Don’t dig into the tender area.
- Waiting it out without changing habits? That’s how acute pain becomes chronic. The Journal of Orthopaedic & Sports Physical Therapy found patients who ignored early symptoms took 3.2 times longer to recover.
- Getting an MRI too soon often leads to unnecessary treatments. If your pain is mild and matches typical patterns, skip the scan.
And here’s a surprising truth: the word “tendinitis” might be outdated. Many chronic cases aren’t truly inflamed-they’re degenerated. Experts now call it “tendinopathy.” That’s why rest and anti-inflammatories don’t always work. You need to rebuild the tissue, not just calm it down.
Real People, Real Results
On Reddit’s r/PhysicalTherapy, users share stories that prove consistency beats quick fixes. One man with chronic shoulder pain thought he had a rotator cuff tear. Turns out, it was bursitis. He stopped lifting weights, started sleeping on his back, and did ice massages daily. Within six weeks, the pain was gone.
Another woman with Achilles tendinitis followed the Alfredson protocol: 180 eccentric heel drops per day for 12 weeks. It was brutal. She cried through the first month. But by week 14, she was back hiking. She tracked her progress with a simple pain scale-no fancy gadgets needed.
And here’s a tip from Arthritis Today readers: modify your workspace. Raise your computer screen to eye level. Use a cushioned mat if you stand all day. Swap out your old sneakers for ones with good arch support. Small changes, big impact.

When to See a Doctor
You don’t need to rush to the clinic for every ache. But if you notice:
- Pain lasting more than two weeks despite rest
- Swelling, redness, or warmth that spreads
- Fever or chills along with joint pain
- Inability to move the joint normally
Then it’s time to get checked. These could be signs of infection, gout, or something more serious.
Also, if you’ve had a cortisone shot and the pain came back within weeks, talk to your doctor. It might mean the root cause wasn’t addressed-like poor posture, muscle weakness, or an underlying joint issue.
What’s New in Treatment
Science is moving beyond just pills and shots. Platelet-rich plasma (PRP) therapy-using your own blood to stimulate healing-is showing promise for chronic tendinitis. One 2023 trial found PRP worked better than cortisone after six months, though it costs about $850 per injection.
Ultrasound-guided injections are now standard because they hit the target 95% of the time, compared to just 70% with blind injections.
And wearable tech? Apple Watch and similar devices are being tested to detect movement patterns that lead to tendinitis before you even feel pain. Early detection could prevent years of discomfort.
How to Prevent It
Prevention is simpler than you think:
- Warm up before activity-even a 5-minute walk helps.
- Strengthen supporting muscles. Strong shoulders protect your tendons. Strong calves protect your Achilles.
- Change positions often. If you kneel, use a pad. If you type, take breaks every 30 minutes.
- Listen to your body. That dull ache? It’s a warning. Don’t push through it.
- Replace worn-out shoes. Flat, hard soles increase stress on tendons and bursae.
The goal isn’t to stop moving-it’s to move smart. Your joints aren’t broken. They’re just asking for a little more care.
Can bursitis and tendinitis happen at the same time?
Yes, and they often do. In fact, about 65% of shoulder pain cases involve both rotator cuff tendinitis and subacromial bursitis. That’s why misdiagnosis is common-treating just one part won’t fix the whole problem. A good physical therapist will assess both structures and tailor exercises accordingly.
Are cortisone shots safe for tendinitis?
They can help with short-term pain, but they’re not ideal for tendons. Injecting cortisone directly into a tendon increases the risk of rupture. That’s why doctors now avoid it for Achilles or rotator cuff tendinitis unless all other options have failed. For bursitis, shots are safer and more effective.
How long does it take to recover from tendinitis?
It depends on how long you’ve had it. Acute tendinitis (under 4 weeks) can improve in 2-6 weeks with rest and gentle movement. Chronic tendinitis (over 3 months) often takes 3-6 months of consistent rehab, especially eccentric strengthening. Patience is key-rushing back to activity is the #1 reason people relapse.
Is heat or ice better for bursitis?
Ice is best in the first few days to reduce swelling. After that, heat can help loosen stiff tissues and improve circulation. But if the area is still swollen or warm to the touch, stick with ice. Heat can make inflammation worse if applied too early.
Can I still exercise with bursitis or tendinitis?
Yes-but you need to modify it. Avoid the movement that causes pain. If your shoulder hurts when you lift overhead, switch to swimming or cycling. Focus on strengthening muscles around the joint without stressing the inflamed area. A physical therapist can design a safe routine. Movement is medicine-but only if it’s the right kind.
Will bursitis or tendinitis go away on its own?
Sometimes, yes-but only if you stop doing what caused it. If you keep kneeling, typing, or lifting the same way, the inflammation will return. These conditions aren’t just about the joint-they’re about your habits. Fix the cause, and the pain usually fades. Ignore it, and it becomes chronic.


Martin Spedding
December 17, 2025 AT 09:13Jessica Salgado
December 19, 2025 AT 05:01Sachin Bhorde
December 20, 2025 AT 06:57Naomi Lopez
December 21, 2025 AT 23:15Kent Peterson
December 23, 2025 AT 22:22Josh Potter
December 25, 2025 AT 07:58Jane Wei
December 26, 2025 AT 16:16Radhika M
December 26, 2025 AT 18:30