COPD Exacerbations: Common Triggers, Warning Signs, and What to Do in an Emergency
 Nov, 18 2025
Nov, 18 2025
When your breathing gets suddenly worse - not just a little, but enough to make you panic - it’s not just a bad day. It’s a COPD exacerbation. For someone living with chronic obstructive pulmonary disease, this isn’t theoretical. It’s a real, dangerous event that can land you in the hospital or worse. Every year in the U.S. alone, over 10 million healthcare visits happen because of these flare-ups. And for many, each one leaves behind permanent damage that doesn’t heal.
What Exactly Is a COPD Exacerbation?
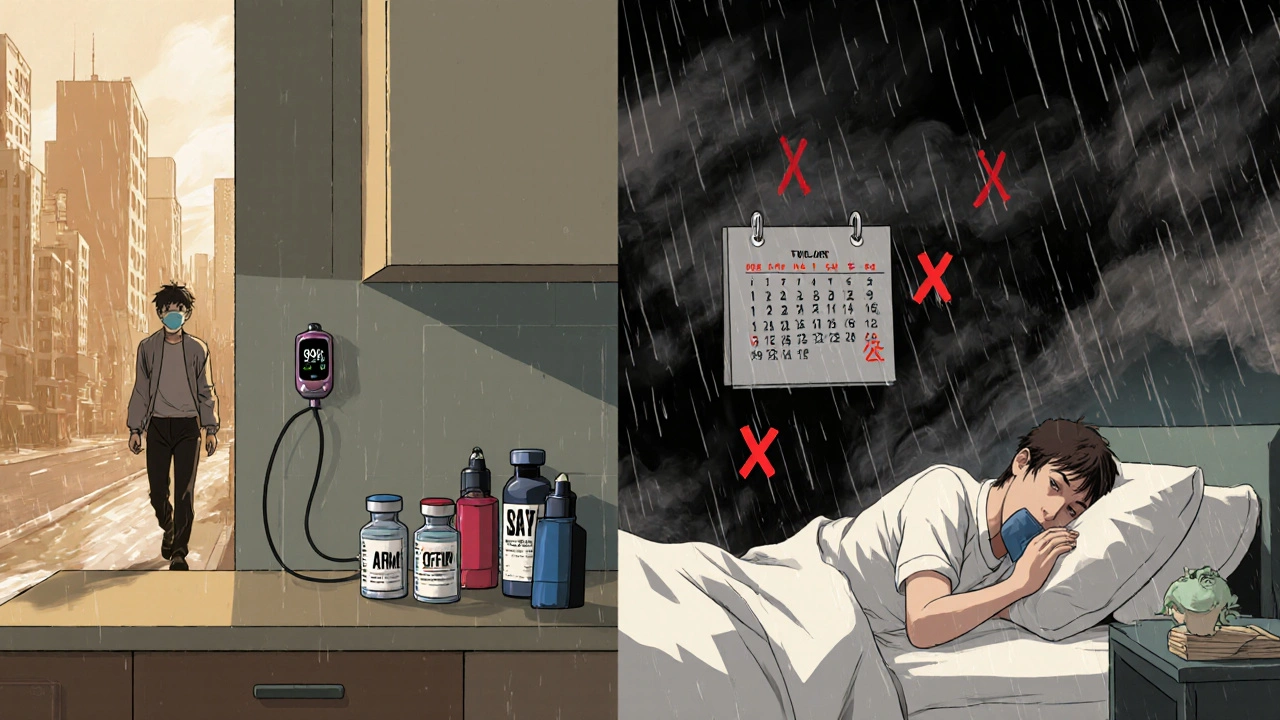
A COPD exacerbation is when your symptoms spike suddenly and stay bad for days or even weeks. It’s more than just feeling winded after climbing stairs. It’s coughing so hard you can’t sleep. It’s waking up gasping because your chest feels tight. It’s your phlegm turning thick, green, or yellow - or even streaked with blood. Your usual inhaler doesn’t help like it used to. You’re more tired than normal. Your lips or fingernails might turn blue. This isn’t just your COPD acting up. It’s your airways inflaming, swelling, and filling with mucus. The muscles around your bronchial tubes tighten. Your lungs can’t push air out properly. That’s why you feel like you’re suffocating even when you’re sitting still. Studies show that after each flare-up, lung function often doesn’t bounce back to where it was before. Over time, this adds up. Each exacerbation chips away at your breathing capacity. That’s why stopping them isn’t optional - it’s essential to staying alive and independent.What Triggers a COPD Flare-Up?
You can’t control everything, but knowing what sets off your flare-ups gives you power. About 75% of all COPD exacerbations are caused by infections. That means germs are your biggest enemy.- Viral infections - Rhinovirus (the common cold), flu, RSV, and even coronaviruses can trigger a flare-up. During the pandemic, many thought COVID-19 would be devastating for COPD patients. Surprisingly, those on regular inhaled medications had less severe outcomes. The meds seem to offer some protection, though we’re still learning why.
- Bacterial infections - Haemophilus influenzae, Streptococcus pneumoniae, and Pseudomonas aeruginosa are common culprits. These often show up when your mucus changes color or gets thicker.
- Environmental irritants - Smoke (even secondhand), strong fumes from cleaning products, perfume, paint, or even cold, dry air can spark inflammation. Air pollution is a silent trigger - especially in cities or during bushfire season, which is all too common in places like Sydney.
- Skipping medications - Missing your daily inhalers or nebulizer treatments makes your airways more vulnerable. It’s not just about feeling okay today. It’s about keeping your lungs protected every single day.
How to Spot a Flare-Up Early
The key to avoiding the ER is catching it early. That’s why you need to know your baseline. On a good day, what’s normal for you? How often do you cough? What color is your mucus? How far can you walk before you need to stop? Write it down. Keep a simple journal - even just a note on your phone. Now, watch for these red flags:- Coughing more than usual, or a change in the sound - deeper, wetter, or more painful
- Mucus that’s darker (yellow, green, or bloody), thicker, or in larger amounts
- Shortness of breath that doesn’t improve with your usual rescue inhaler
- Wheezing or chest tightness that’s worse than normal
- Fever, chills, or feeling unusually weak or dizzy
- Difficulty sleeping because you can’t catch your breath
- Swelling in your ankles or feet - this can mean your heart is struggling too

Emergency Treatment: What Happens in the Hospital?
If you’re struggling to breathe, your oxygen level is below 90%, or your lips are turning blue - don’t wait. Call emergency services. This is life-threatening. In the hospital, doctors focus on three things:- Restoring oxygen - You’ll get supplemental oxygen through a mask or nasal prongs. Too much oxygen can be dangerous for some COPD patients, so it’s carefully controlled.
- Opening your airways - You’ll get stronger doses of bronchodilators (like albuterol) through a nebulizer. Steroids (like prednisone) are given orally or intravenously to reduce swelling in your lungs.
- Treating infection - If there’s evidence of bacteria (thick green mucus, fever), you’ll get antibiotics. Common ones include amoxicillin-clavulanate, doxycycline, or azithromycin. If it’s viral, antibiotics won’t help - but steroids and oxygen still will.
What You Can Do at Home (Before It Gets Bad)
You don’t have to wait for an emergency. Most flare-ups can be managed at home - if you act fast. Work with your doctor to create a COPD Action Plan. This isn’t a suggestion. It’s your personal survival guide. It should include:- When to increase your rescue inhaler use
- When to start oral steroids (and how much)
- When to begin antibiotics (if you’ve been prescribed them for this purpose)
- When to call your doctor
- When to go to the ER
- Extra rescue inhaler (never let it run out)
- Oral steroids (if prescribed)
- Thermometer
- Portable pulse oximeter (to check oxygen levels at home)
- Hydration - drink water, even if you’re not thirsty. Thin mucus is easier to clear.
Prevention: The Only Real Long-Term Solution
The best treatment for a COPD exacerbation is not having one at all.- Get vaccinated - Every year: flu shot. Once or twice: pneumococcal vaccine. Ask your doctor which ones you need.
- Take your maintenance meds daily - Even when you feel fine. Inhaled corticosteroids and long-acting bronchodilators reduce inflammation and keep your airways open.
- Avoid triggers - No smoking. No vaping. Stay indoors on high-pollution days. Use air purifiers. Avoid strong scents. Wear a mask in crowded places during cold and flu season.
- Exercise - Walking 20 minutes a day improves lung efficiency and reduces flare-up risk. Pulmonary rehab programs are proven to cut hospitalizations by nearly half.
- Monitor your health - Weigh yourself daily. A sudden 2-3 kg weight gain can mean fluid buildup - a sign your heart is under stress.
What Happens If You Ignore It?
Ignoring a flare-up doesn’t make it go away. It makes it worse. Each untreated exacerbation can permanently reduce your lung function by 5-10%. That might not sound like much, but over five years, that’s 30-50% of your breathing capacity gone. You’ll need more oxygen. You’ll need help walking. You might stop leaving the house. And the risk of death rises sharply after each episode. One study found that one in five people who are hospitalized for a COPD flare-up die within a year. This isn’t fearmongering. It’s fact. COPD was the fourth leading cause of death in 2019. And most of those deaths were linked to untreated or poorly managed exacerbations.Final Thought: You’re Not Powerless
COPD is a tough disease. But flare-ups aren’t inevitable. You have tools. You have knowledge. You have a plan - if you’ve made one. Start today. Write down your baseline symptoms. Get your vaccines. Keep your inhalers full. Learn your warning signs. Talk to your doctor about an action plan. The next time your chest tightens or your cough worsens, don’t wait. Don’t hope it passes. Act. Because every minute counts when your lungs are fighting for air.What are the first signs of a COPD exacerbation?
The earliest signs include increased coughing, more mucus than usual, mucus that’s thicker or darker in color (yellow or green), worsening shortness of breath during normal activities, and feeling more tired than usual. If these symptoms last more than two days, it’s likely a flare-up.
Can COPD exacerbations be prevented?
Yes, many can be prevented. The most effective steps include getting annual flu and pneumonia vaccines, taking prescribed maintenance inhalers daily, avoiding smoke and air pollution, washing hands often to prevent infections, and following a personalized COPD Action Plan developed with your doctor.
When should I go to the hospital for a COPD flare-up?
Go to the hospital if you’re struggling to breathe even while resting, your lips or fingernails turn blue, your oxygen level drops below 90% (if you have a pulse oximeter), you’re confused or drowsy, or your rescue inhaler isn’t helping. These are signs of a medical emergency.
Do antibiotics help with all COPD exacerbations?
No. Antibiotics only help if the flare-up is caused by a bacterial infection - usually indicated by thick, colored mucus, fever, or worsening symptoms after a cold. Viral infections (like colds or flu) don’t respond to antibiotics. Your doctor will decide based on your symptoms and medical history.
How long does a COPD exacerbation last?
Most flare-ups last 7 to 14 days, but some can drag on for weeks. Even after symptoms improve, lung function may not return to normal for up to eight weeks. That’s why each exacerbation can cause lasting damage.
Can using my inhaler too much during a flare-up be dangerous?
Using your rescue inhaler as directed during a flare-up is safe and necessary. But if you’re using it more than every 4 hours for more than a day, or if it’s not helping, that’s a sign you need stronger treatment - like steroids or medical care. Don’t delay seeking help just because you’re afraid of overusing your inhaler.
Is it safe to fly with COPD during flare-up season?
Flying during an active flare-up is risky. Lower oxygen levels in airplane cabins can make breathing much harder. If you’re planning to fly, talk to your doctor first. You may need supplemental oxygen on the flight. Avoid flying if you’re currently having symptoms or just recovering from a flare-up.


Dana Dolan
November 20, 2025 AT 16:17Just had my third flare-up this winter. Didn’t think the new inhaler combo would help, but damn-it actually did. I started using it religiously after reading this. No more panic attacks when the air turns crisp.
Also, I keep a little notebook on my fridge with my baseline symptoms. Changed everything.
seamus moginie
November 21, 2025 AT 14:51This is the most accurate, no-nonsense breakdown of COPD exacerbations I’ve ever read. I’ve been telling my patients for years that skipping meds is like leaving your front door open during a hurricane. Yet they still do it. Why? Because they think they’re fine until they’re not.
Doctors need to stop sugarcoating this. It’s not ‘bad days.’ It’s slow suicide with a prescription.
Ellen Calnan
November 23, 2025 AT 02:38I used to think COPD was just ‘old people breathing hard.’ Then my mom got diagnosed at 58. She’s still walking three miles a day, but now she measures her oxygen before coffee. Every. Single. Morning.
It’s not about fear. It’s about respect. For your lungs. For your family. For the fact that you’re still here, and that’s a gift.
I started carrying an extra inhaler in my purse. Just in case. You never know when the air turns thick with smoke from a wildfire 200 miles away. And suddenly-you’re gasping.
I used to think ‘stay calm’ was the advice. Now I know: act fast. Calm comes after you’ve taken the first step.
There’s power in preparation. Not in prayer. In planning.
I cried reading this. Not because it’s scary. Because it’s true. And someone finally said it without fluff.
Thank you.
My mom’s 70 now. Still stubborn. Still alive. And I’m still learning how to love her without smothering her.
This post? It’s a lifeline.
Richard Risemberg
November 23, 2025 AT 07:01Let me tell you about the guy who refused to get the flu shot because ‘it’s just a cold.’ He’s in a nursing home now, on 24/7 oxygen, and his wife says he hasn’t walked to the mailbox in 18 months.
Meanwhile, my buddy Frank-he’s 72, smoked for 40 years, but he gets his shots, takes his meds, and walks 10K steps every day. He just got back from a cruise. No issues.
It’s not about luck. It’s about discipline. And discipline is just habit with teeth.
Don’t wait for your lungs to beg you to listen. They don’t yell. They whisper. And by the time you hear them? It’s too late.
So yeah. Get the shot. Take the pill. Walk the damn block. Your future self will high-five you.
And if you’re reading this and thinking ‘I’ll start tomorrow’-you’re already behind. Start now. Right now. Put the phone down. Breathe. Then move.
Andrew Montandon
November 24, 2025 AT 02:03Important note: Pulse oximeters are NOT toys. Get one. Use it. Know your numbers. Mine says 92% on a good day. If it drops below 88%, I call my doc. No waiting. No ‘maybe it’ll pass.’
Also, hydration isn’t optional. I drink a full liter of water before bed. Why? Thick mucus = blocked airways = panic. Water thins it. Simple.
And yes-I keep my rescue inhaler in my coat pocket, my car, and my nightstand. Triple redundancy. Because when you’re gasping, you don’t want to be hunting for it.
Also-air purifiers are a game-changer. I got a cheap one from Amazon. It’s not fancy, but it cuts dust, pollen, and even some VOCs. My cough dropped by 60% in two weeks.
Don’t underestimate clean air. It’s not a luxury. It’s medicine.
And if you’re skipping your maintenance inhaler because you ‘feel fine’-you’re playing Russian roulette with your lungs. Stop it.
And for the love of God-don’t let your kids smoke around you. Even if they ‘only do it outside.’ It clings. It lingers. It kills.
Sam Reicks
November 25, 2025 AT 11:35So let me get this straight-you’re telling me that if I just take my inhalers and get a flu shot, I won’t die from COPD? That’s it? No hidden cure? No secret government drug? No miracle supplement? You’re seriously selling this as a solution?
I’ve read studies that say oxygen therapy accelerates lung decay. And that antibiotics are overprescribed. And that the ‘action plan’ is just a way for Big Pharma to keep you buying meds.
What if the real problem is air pollution? Or vaccines? Or 5G? I mean, why do only some people with COPD flare up? Why not everyone?
I’ve been tracking my symptoms since 2015. I’ve noticed a pattern: flare-ups spike right after the CDC releases new guidelines. Coincidence? I think not.
Also, my neighbor’s cat sneezed near me last week. I had a flare-up three days later. Coincidence? I think not.
Maybe the real enemy isn’t the virus. Maybe it’s the system.
And if you’re telling me to ‘walk 20 minutes a day’-I’ve got a 200-pound dog who doesn’t even want to go outside. So what’s your solution for me?
Just saying-don’t give me platitudes. Give me truth.
Or at least admit you don’t have all the answers.
Reema Al-Zaheri
November 26, 2025 AT 05:33My father passed away last year from a COPD exacerbation. He refused to use his pulse oximeter because he said, 'I know how I feel.' He didn't want to be a burden. He didn't want to 'overreact.'
He died in his sleep. No warning. No ambulance. No last words.
This article is the most comprehensive guide I've ever read on the subject. I wish I had it three years ago.
I now keep his inhalers, his oximeter, and his action plan on my phone. I check them every morning. I don't wait for symptoms. I prevent them.
Do not make the same mistake. Even if you feel fine. Even if you think it's 'just a cough.'
Prevention is not optional. It is the only thing that gives you time.
And time is the one thing you can't get back.
Michael Salmon
November 27, 2025 AT 21:36Wow. Another feel-good, corporate-approved COPD pamphlet. Let me guess-this was written by a pharmaceutical rep with a marketing degree?
Did you mention that 70% of COPD patients are on Medicaid? Or that most can’t afford the ‘maintenance inhalers’ you’re pushing? Or that pulmonary rehab costs $10,000 a year and isn’t covered in half the states?
You talk about ‘action plans’ like they’re free, easy, and accessible. They’re not.
You talk about vaccines like they’re magic bullets. But what about the people who got the flu shot and still ended up in the ICU?
And don’t even get me started on ‘walk 20 minutes a day.’ Try walking when your legs are weak, your heart’s racing, and your oxygen’s at 86%.
This isn’t advice. It’s victim-blaming dressed up as hope.
Real talk: The system is rigged. The meds are expensive. The doctors are overworked. And the patients? They’re just trying to survive the next hour.
Stop pretending this is about willpower. It’s about poverty, access, and neglect.
Joe Durham
November 29, 2025 AT 01:22I just wanted to say thank you to everyone who’s shared their stories here.
To Dana-your notebook idea? I’m stealing it.
To Richard-your ‘habit with teeth’ line? That’s going on my fridge.
To Reema-I’m so sorry for your loss. Your words hit hard.
To Sam-I hear you. The system is broken. And you’re not wrong.
But here’s what I’ve learned: You don’t have to fix the whole system to save your own life.
Maybe you can’t afford the inhaler. But can you ask for samples? Can you call your pharmacy and ask about patient assistance programs?
Maybe you can’t walk 20 minutes. But can you stand up and stretch for 2 minutes? Can you sit by the window and breathe slow for 60 seconds?
Small things matter.
And you’re not alone.
I’ve been living with COPD for 12 years. I’ve had five flare-ups. I’ve been hospitalized twice.
I’m still here.
Not because I’m strong.
Because I had people who cared enough to tell me the truth.
And now I’m telling you: You can still live. Even if it’s hard. Even if it’s messy. Even if the system lets you down.
Start small.
Stay close to people who get it.
And never, ever stop asking for help.
Because you’re worth it.