Deprescribing Frameworks: How to Safely Reduce Medications and Reduce Side Effects
 Nov, 19 2025
Nov, 19 2025
Medication Review Tool
This tool helps you identify medications that may be candidates for deprescribing based on evidence-based guidelines. Remember: Never stop taking any medication without consulting your healthcare provider.
Medication Safety Assessment
Enter your medications and click "Review Medications" to see potential candidates for deprescribing.
How to Proceed
Based on your assessment:
- Ask your doctor: "Is this still necessary?" and "What would happen if I stopped it?"
- Request a medication review with a pharmacist (many insurance plans cover this)
- Consider a 2-4 week follow-up visit after starting any deprescribing
- Track your symptoms during any tapering process
Every year, millions of older adults take medications that no longer help them-and may be hurting them. It’s not laziness or neglect. It’s often just how medicine works: a drug gets added for one condition, then another, then another. Over time, the list grows. And so do the side effects: dizziness, confusion, falls, stomach bleeds, fatigue. Many patients don’t even realize their symptoms are drug-related. That’s where deprescribing comes in-not just stopping pills, but doing it safely, systematically, and with purpose.
What Deprescribing Really Means
Deprescribing isn’t the opposite of prescribing. It’s not about cutting drugs just because they’re old or numerous. It’s a careful, evidence-based process of reviewing each medication to ask: Is this still helping, or is it now doing more harm than good? The goal isn’t fewer pills for the sake of fewer pills. It’s better health, fewer side effects, and improved quality of life.According to the World Health Organization, about 40% of older adults worldwide are taking five or more medications at once-a situation called polypharmacy. And it’s dangerous. A 2023 study from the American Geriatrics Society found that inappropriate polypharmacy contributes to 30% of hospital admissions in people over 65. Many of those admissions could have been avoided if those medications had been reviewed and, when needed, safely reduced.
Deprescribing frameworks were developed to bring structure to this process. Before 2010, doctors often didn’t know how to stop medications safely. Now, there are clear protocols for the most common high-risk drugs: proton-pump inhibitors (PPIs), benzodiazepines, antipsychotics, blood sugar medications, and opioids. Each framework follows the same basic steps: identify the drug, check if it’s still needed, taper it slowly, and monitor for changes.
The Shed-MEDS Framework: A Proven Method
One of the most validated deprescribing tools is called Shed-MEDS. It stands for:- Best Possible Medication History-get a complete, accurate list of everything the patient is taking, including over-the-counter drugs and supplements.
- Evaluate-use guidelines like STOPP/START or the Beers Criteria to flag drugs that may be inappropriate for older adults.
- Deprescribing Recommendations-prioritize which drugs to reduce first based on risk, benefit, and patient goals.
- Synthesis-create a clear plan with the patient and care team, including tapering schedules and warning signs to watch for.
A 2023 JAMA Internal Medicine trial tested Shed-MEDS in 372 older adults in post-acute care. The results were striking. Patients in the deprescribing group went from an average of 11.3 medications down to 9.5 at discharge-and still had 1.6 fewer meds at 90 days. The best part? There was no increase in hospital visits or adverse events. The control group, which got usual care, didn’t see any change in their medication count.
Which Medications Are Most Often Overused?
Not all drugs are created equal when it comes to deprescribing. Some carry much higher risks than others. Here are the top five classes targeted by current guidelines:- Proton-pump inhibitors (PPIs)-like omeprazole or pantoprazole. Many people take them for heartburn, but most don’t need them long-term. Stopping them safely can reduce risks of kidney damage, bone fractures, and infections.
- Benzodiazepines and sleep aids-drugs like lorazepam, diazepam, or zolpidem. These increase fall risk and confusion in older adults. Tapering them slowly over 4-8 weeks can improve alertness and balance.
- Antipsychotics-often prescribed for dementia-related agitation, even though they’re not approved for that use. These drugs can cause tremors, stiffness, and even sudden death. Deprescribing them often leads to better behavior, not worse.
- Antihyperglycemics-medications like glyburide or insulin for diabetes. Tight blood sugar control isn’t always better in older adults. Reducing these can prevent dangerous low blood sugar episodes.
- Opioid painkillers-long-term use increases risk of addiction, constipation, and respiratory issues. For chronic non-cancer pain, non-drug options and lower doses often work better.
Each of these has a published deprescribing algorithm on deprescribing.org. These aren’t vague suggestions-they’re step-by-step guides with specific tapering schedules and monitoring recommendations.
Why It’s Hard to Do in Practice
Even with clear tools, deprescribing isn’t easy. Most primary care visits last only 7-10 minutes. Trying to review 12 medications in that time? Nearly impossible.Pharmacists are the secret weapon. Studies show deprescribing success rates jump 35-40% when pharmacists are involved. They have the time to sit with patients, explain why a drug might be stopped, and manage the tapering process. But most clinics don’t have pharmacists on staff-or don’t let them lead the process.
Electronic health records (EHRs) aren’t helping much either. Only 32% of clinicians say their EHR system supports deprescribing. Most systems are built to remind doctors to add medications, not to question if they’re still needed. Some forward-thinking health systems have flipped the script: instead of letting doctors prescribe a risky drug easily, they make them actively choose to override a warning. That small design change has reduced inappropriate prescribing by up to 40% in pilot programs.
The Human Side: Patient Fear and Trust
Stopping a medication after 10 or 20 years isn’t just a clinical decision-it’s emotional. Many patients believe a pill is a lifeline. If they’ve been taking it since their 50s, they think it’s keeping them alive.A 2022 study found that 65% of older adults felt relieved after reducing their meds. But 22% were anxious-even terrified. One woman stopped her daily statin after her pharmacist walked her through the evidence: her cholesterol was normal, her risk of heart disease was low, and she’d been experiencing muscle pain for years. She cried when she realized the pain wasn’t just aging-it was the drug.
But others worry about rebound symptoms. What if the heartburn comes back? What if they can’t sleep? That’s why tapering matters. You don’t just flip a switch. You reduce slowly, watch closely, and give patients control. A good deprescribing plan includes a written plan, a contact number for questions, and a follow-up visit within 2-4 weeks.
What’s Changing in 2025?
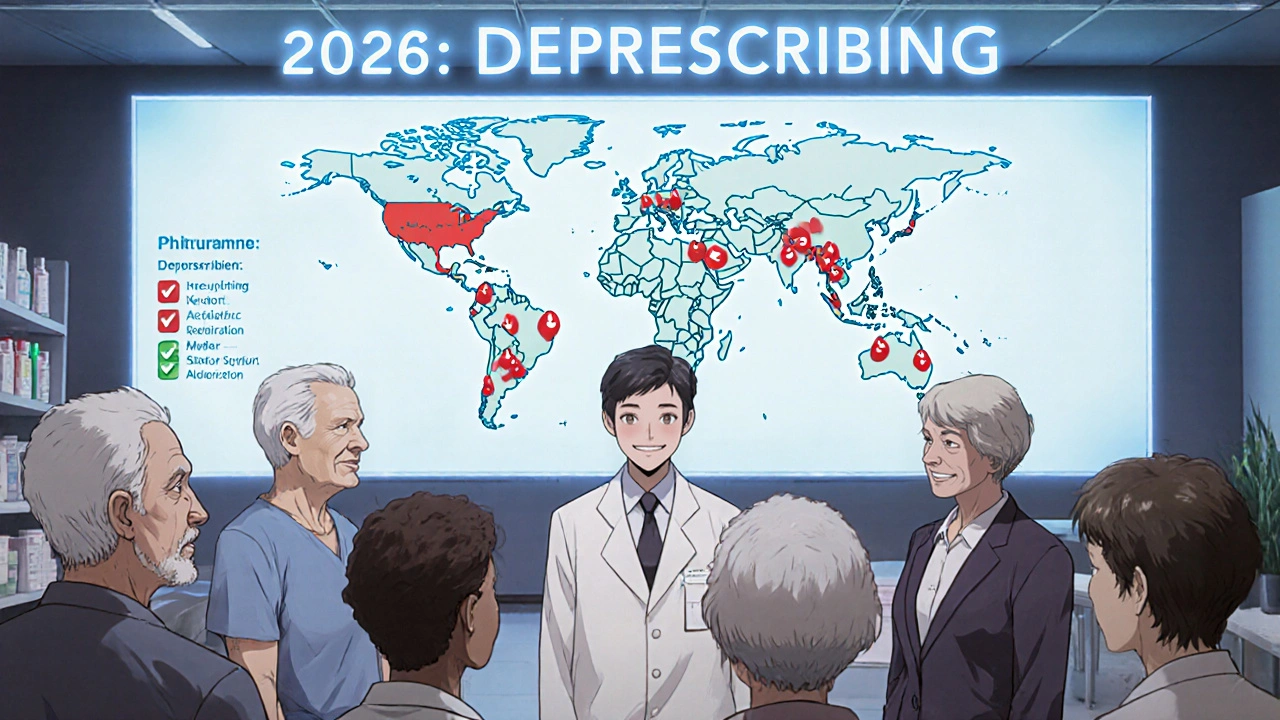
The tide is turning. In June 2024, the American Medical Association issued its first official policy: physicians must routinely review all medications for appropriateness. That’s a big deal-it turns deprescribing from a nice idea into a professional obligation.Medicare is catching up too. Starting in 2026, doctors will be scored on how often they reduce inappropriate medications. That means clinics will need systems, training, and time to do this right.
Researchers are also working on AI tools that scan EHRs and flag patients who might benefit from deprescribing. These tools look at age, diagnoses, drug combinations, lab results, and even pharmacy refill patterns to suggest candidates. One pilot at a large hospital system flagged 1,200 patients in six months-87% of whom were on at least one high-risk medication.
By 2030, experts predict deprescribing checks will be as routine as checking blood pressure during annual wellness visits. The data is clear: reducing unnecessary meds saves money, prevents hospitalizations, and improves daily life.
What Patients Can Do Today
You don’t have to wait for your doctor to bring it up. Here’s what you can do:- Make a complete list of everything you take-prescriptions, vitamins, herbal supplements, OTC painkillers. Include doses and why you take them.
- Ask your doctor: “Is this still necessary?” and “What would happen if I stopped it?”
- Request a medication review with a pharmacist. Many insurance plans cover this service.
- Don’t stop anything cold turkey. Ask for a tapering plan if you’re thinking about quitting.
- Track how you feel after reducing a drug. Did your energy improve? Did the dizziness go away? Write it down.
Deprescribing isn’t about giving up treatment. It’s about getting back to what matters: feeling well, moving without pain, sleeping without pills, and living without the burden of too many medications.
Is deprescribing safe?
Yes, when done properly. Multiple studies, including a 2023 JAMA trial with over 370 older adults, show that deprescribing reduces medication burden without increasing hospitalizations or adverse events. The key is doing it slowly, with monitoring, and based on individual needs-not just stopping everything at once.
Can I stop my medication on my own?
No. Some medications, like benzodiazepines, antidepressants, or steroids, can cause serious withdrawal symptoms if stopped abruptly. Even if you think a drug isn’t helping, always talk to your doctor or pharmacist first. They can create a safe tapering plan tailored to your health.
What if I’m afraid my symptoms will come back?
That’s a common concern-and it’s why deprescribing includes a monitoring phase. Your care team will help you track symptoms during the taper. If something returns, you can restart the medication. But in many cases, the original symptom was either mild, unrelated to the drug, or already improving on its own.
Who should consider deprescribing?
Anyone taking five or more medications, especially older adults, those with limited life expectancy, or those experiencing side effects like dizziness, confusion, fatigue, or falls. But even younger people on long-term PPIs, sleep aids, or painkillers can benefit from a review.
Are there tools I can use at home?
Yes. deprescribing.org offers free, evidence-based algorithms for common medications like PPIs, benzodiazepines, and antipsychotics. The American Geriatrics Society’s Beers Criteria and STOPP/START guidelines are also publicly available. These aren’t DIY tools, but they can help you ask better questions during your next doctor visit.
Final Thoughts
Medications save lives. But they also cause harm-especially when they’re taken too long, at too high a dose, or without a clear purpose. Deprescribing isn’t about removing care. It’s about refining it. It’s about listening to the body, not just the prescription pad. And it’s about giving people back their time, their energy, and their peace of mind.The future of medicine isn’t just adding more drugs. It’s knowing when to let go.


Ravinder Singh
November 19, 2025 AT 09:44Wow, this is the kind of post I wish I’d found 5 years ago when my dad was on 14 meds and barely able to walk. 🙏 We didn’t know half his dizziness was from benzos. Once we tapered him off slowly with his pharmacist’s help? He started gardening again. No magic, just common sense. Thanks for laying this out so clearly.
Russ Bergeman
November 20, 2025 AT 10:04Okay, but… isn’t this just ‘medication hoarding’ by another name? Like, if it’s prescribed, it’s ‘necessary,’ right? I mean, who even decides what’s ‘inappropriate’? Some algorithm? 😅
Dana Oralkhan
November 21, 2025 AT 19:32I’ve seen this firsthand with my mom. She was on PPIs for 12 years because ‘it’s just heartburn.’ Turns out, she was having acid reflux because she ate right before bed-not because her stomach made too much acid. Stopping it? She felt like a new person. But it took months of gentle tapering. Please, if you’re on long-term meds, don’t just assume they’re helping. Ask. Ask again. Ask a pharmacist.
Jeremy Samuel
November 21, 2025 AT 20:59deprescribing? more like de-caring. you wanna stop meds? fine. but what if you’re wrong? people die from this stuff. i mean, come on. if your doc says take it, take it. stop being a lab rat.
Destiny Annamaria
November 23, 2025 AT 10:09OMG I JUST REALIZED MY AUNT IS ON 8 MEDS AND SHE’S 78 AND STILL DANCES AT FAMILY WEDDINGS 😱 I’m gonna send her this post. She needs to know she doesn’t have to feel like a walking pharmacy. Also, anyone know if Walgreens does med reviews? 🤔
Ron and Gill Day
November 24, 2025 AT 17:03This is textbook medical socialism. You’re telling people to stop taking life-saving drugs because some ‘framework’ says so? Who funded this? Big Pharma hates this. You’re endangering lives under the guise of ‘quality of life.’ Pathetic.
Alyssa Torres
November 26, 2025 AT 08:59I cried reading this. My grandma was on antipsychotics for ‘agitation’-she just missed her husband. They didn’t try talking to her. They just drugged her. When we finally stopped it? She started singing old Bollywood songs again. No more tremors. No more staring into space. Just… her. This isn’t about reducing meds. It’s about restoring humanity. Thank you.
Summer Joy
November 26, 2025 AT 14:40So… you’re saying my 80-year-old uncle who’s been on statins since 1998 should just quit? 😭 What if he drops dead tomorrow? Who’s gonna be responsible? The pharmacist? The algorithm? I’m not signing up for that drama. This is dangerous. Someone’s gonna get sued. I can feel it.
Aruna Urban Planner
November 27, 2025 AT 13:35From a systems perspective, the structural inertia within primary care workflows is the true bottleneck. The cognitive load of polypharmacy review exceeds the temporal bandwidth of standard visit protocols. Without embedded clinical decision support and interprofessional collaboration-particularly with pharmacists-the Shed-MEDS framework remains theoretically elegant but operationally under-resourced. We need reimbursement reform, not just guidelines.
Nicole Ziegler
November 27, 2025 AT 22:00My mom stopped her sleep meds last year… and now she sleeps like a baby without them 😴✨ I used to think she needed them… turns out she just needed quiet and a cooler room. This post made me realize how much we assume meds are the answer. 🤯
Bharat Alasandi
November 28, 2025 AT 01:18Bro, I saw this in my village back home. Old man took 10 pills every day for ‘blood pressure’ and ‘joint pain’ and ‘sleep.’ His son took him to a clinic that does med reviews. Now he’s on 3. Walks 5km every morning. Says he feels ‘lighter than his chai cup.’ This ain’t science fiction. It’s common sense with data.
Kristi Bennardo
November 29, 2025 AT 09:23This is a dangerous precedent. The medical profession is being undermined by layperson-driven ‘medication audits.’ If patients are empowered to question every prescription, we will descend into a chaos of self-diagnosis and noncompliance. This is not patient-centered care-it’s patient-led recklessness.
Shiv Karan Singh
November 29, 2025 AT 22:42lol deprescribing? more like ‘let’s get people off meds so they die faster.’ what’s next? telling diabetics to stop insulin? this is the dumbest thing i’ve read all week. people are dying from this nonsense. you’re not a doctor. stop giving advice.
Ravi boy
November 30, 2025 AT 12:06my uncle stopped his ppi and his heartburn came back… but he said it was worth it cause he stopped feeling foggy. he’s still alive. so… maybe it works? idk. just saying.