Diarrhea: Understanding Acute vs. Chronic and When Antimotility Drugs Help
 Dec, 31 2025
Dec, 31 2025
Diarrhea isn’t just a bad day at the bathroom-it’s a signal your body is trying to tell you something. Whether it’s a sudden bout after eating bad sushi or months of unpredictable loose stools, the difference between acute and chronic diarrhea changes everything about how you handle it. And knowing when to reach for an antimotility drug like loperamide-or when to avoid it-can make the difference between relief and serious harm.
What Exactly Is Diarrhea?
Diarrhea means passing three or more loose or watery stools in a day. It’s not a disease itself, but a symptom. The real clue isn’t just frequency-it’s consistency. Stools that are watery, unformed, or urgent are the hallmark. Doctors don’t weigh every stool (though technically, diarrhea means more than 200-300 grams per day), they look at what you’re seeing in the toilet. That’s enough to diagnose it.Acute Diarrhea: Sudden, Short, and Usually Harmless
If your diarrhea started yesterday and you’re on day 3, you’ve got acute diarrhea. By definition, it lasts 14 days or less. Most cases-70% to 80% in places like the U.S. and Australia-are caused by viruses. Rotavirus used to be the big one in kids, but vaccines have cut those cases by 40-60%. Now, norovirus and other bugs are more common. Bacteria like Salmonella, Campylobacter, or E. coli cause 10-20% of cases, usually from undercooked meat or contaminated water. Parasites like Giardia show up in 5-10%, often after hiking, camping, or traveling to areas with unsafe water. The good news? Most acute diarrhea clears up on its own in 3-7 days. You won’t need antibiotics. In fact, using them unnecessarily can make things worse by killing off good gut bacteria and increasing the risk of antibiotic-resistant infections.Chronic Diarrhea: When It Won’t Go Away
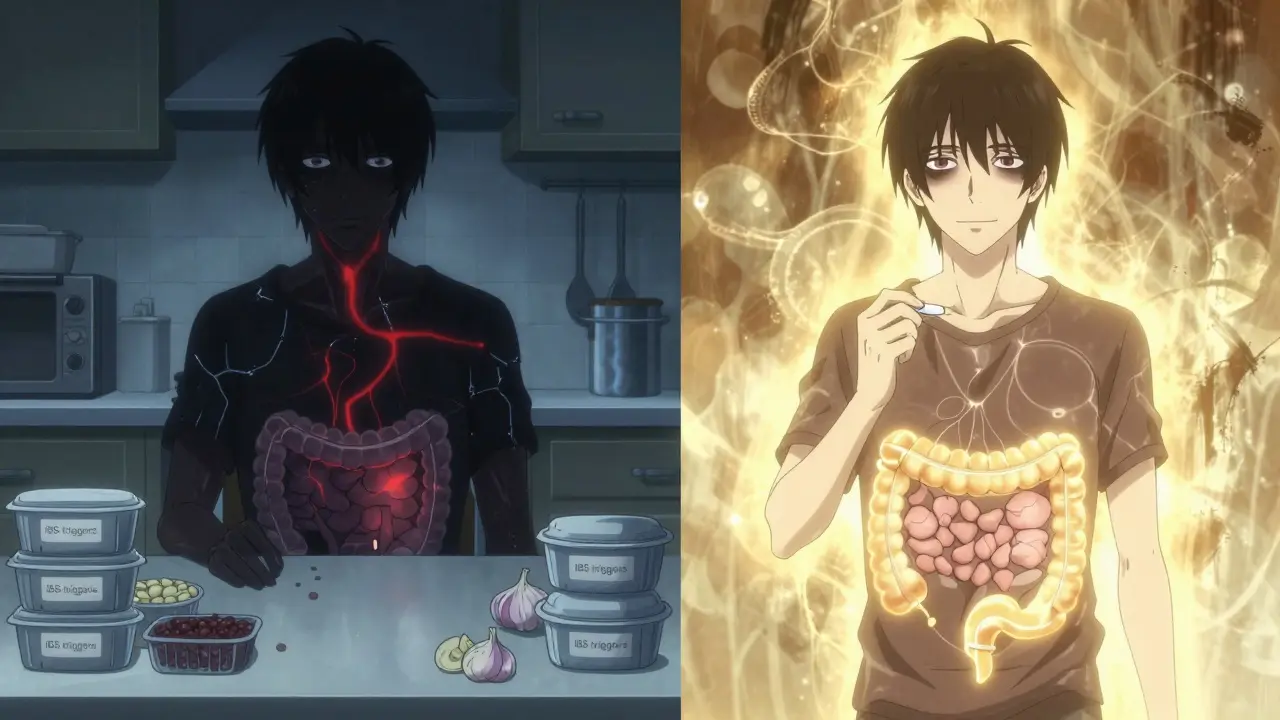
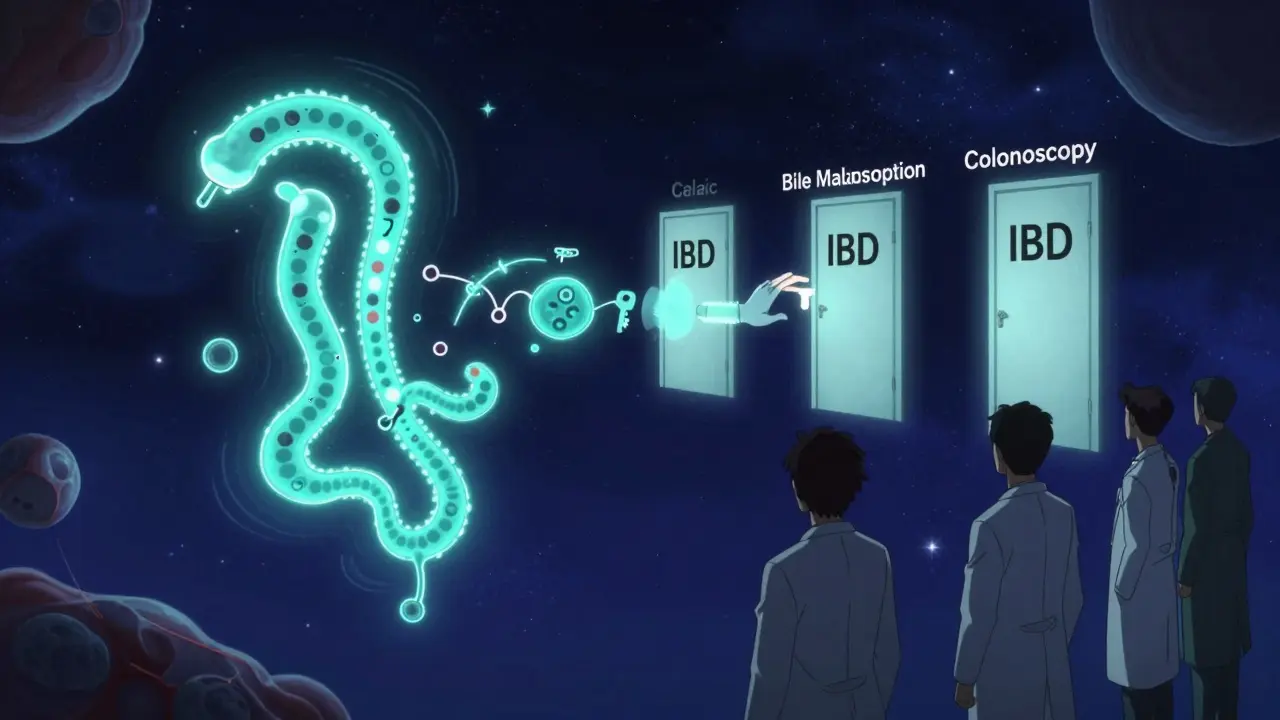
If you’ve had loose stools for more than 14 days, it’s chronic. And this is where things get serious. Only about 5% of adults in developed countries deal with this, but it’s not something to ignore. Unlike acute diarrhea, chronic diarrhea is rarely caused by an infection. Instead, it’s usually tied to long-term conditions:- Irritable Bowel Syndrome (IBS-D): Affects 10-15% of people globally. It’s functional-meaning no visible damage, but your gut is overly sensitive. Stress, food triggers, and gut-brain communication play big roles.
- Inflammatory Bowel Disease (IBD): Includes Crohn’s disease and ulcerative colitis. These cause inflammation in the gut lining, leading to bloody stools, weight loss, and fatigue. Around 1.6 million Americans have IBD.
- Bile Acid Malabsorption: Happens in 25-30% of people after gallbladder removal. Bile that should be recycled ends up in the colon, pulling water and causing watery diarrhea.
- Celiac Disease: An autoimmune reaction to gluten. Often mistaken for IBS-40% of celiac cases are misdiagnosed as such before testing.
- Medications: Antibiotics, metformin, laxatives, and even some heart or cancer drugs can trigger chronic diarrhea.
How Do You Know If It’s Acute or Chronic?
The symptoms overlap, but clues matter:- Acute: Sudden onset. Often with cramps, nausea, vomiting, maybe fever. No weight loss. Feels like you’ve been hit by a bug.
- Chronic: Persistent. May come and go, but never fully disappears. Often linked to weight loss, bloating, nocturnal diarrhea (waking up at night to go), or fatty, oily stools (steatorrhea). Nighttime symptoms are a red flag-it suggests something structural, not just a virus.
Antimotility Agents: Loperamide and Beyond
Antimotility drugs slow down your gut. The most common is loperamide (Imodium). It works by reducing muscle contractions in the intestines, so stool moves slower and becomes firmer. It’s effective-for both acute and chronic cases. For acute diarrhea: Start with 4mg after the first loose stool, then 2mg after each subsequent loose stool. Don’t exceed 16mg in 24 hours. It helps you feel better faster, but doesn’t cure the infection. For chronic diarrhea: Many people with IBS-D find loperamide life-changing. One patient reported going from 10 bowel movements a day to just 2-3 after taking 2mg before meals. It lets people return to work, travel, and social life. But here’s the catch: Don’t use loperamide if you have bloody diarrhea or a high fever. That’s a sign of a serious bacterial infection like Shiga-toxin E. coli or C. difficile. Slowing down your gut in those cases traps toxins inside, raising your risk of toxic megacolon or hemolytic uremic syndrome-both life-threatening. The FDA warns against misuse. Between 2011 and 2021, over 1,200 cases of loperamide abuse were reported, with 57 deaths. People took massive doses (up to 100mg a day) trying to get high or manage opioid withdrawal. That’s why loperamide packages are now limited to 48mg per box in the U.S. Bismuth subsalicylate (Pepto-Bismol) is another option. It reduces diarrhea and has mild antibacterial effects. Safe for short-term use, but avoid if you’re allergic to aspirin or on blood thinners.What About Oral Rehydration?
No matter the cause, hydration is non-negotiable. Especially for kids, the elderly, or anyone vomiting alongside diarrhea. The WHO’s oral rehydration solution (ORS) is the gold standard: 2.6g sodium chloride, 2.9g trisodium citrate, 1.5g potassium chloride, and 13.5g glucose per liter of water. It’s cheap, effective, and cuts death rates by 93% in low-resource settings. You don’t need fancy drinks. A homemade version-1 liter of clean water, 6 tsp sugar, and half a tsp salt-works in a pinch. But avoid sugary sodas or fruit juices. They make diarrhea worse by pulling more water into the gut.When to Skip the Pills and Fix the Root Cause
For chronic diarrhea, treating the symptom isn’t enough. You need to find the cause.- IBS-D: Try a low-FODMAP diet. Studies show 50-75% of people improve after 6-8 weeks under a dietitian’s guidance. Foods like onions, garlic, beans, and certain fruits trigger symptoms.
- Bile acid diarrhea: Cholestyramine or colesevelam (bile acid sequestrants) bind excess bile in the gut. Often works wonders.
- Celiac disease: A simple blood test and biopsy can confirm it. Go gluten-free-and symptoms often vanish.
- Medication-induced: Talk to your doctor. Maybe your metformin dose can be lowered, or you can switch antibiotics.
What Patients Really Say
Online forums reveal real struggles. One Reddit user wrote: "I went to 5 doctors over 18 months. They all said it was IBS. I had bloody stools and lost 15kg. Turned out to be Crohn’s." Another shared: "Loperamide saved me at first. But after 6 months, I was taking 8mg a day just to feel normal. I felt addicted-and scared to stop." And it’s true: many patients feel dismissed. Chronic diarrhea is invisible. People don’t understand why you can’t just "deal with it." But the delay in diagnosis is real-68% of patients wait six months or longer for answers.What’s New in 2025?
The WHO updated its ORS formula in 2022 with lower sodium and glucose levels. It reduces stool output by 25% compared to the old version. In 2023, the FDA approved a new extended-release loperamide designed to make abuse harder. It’s not yet widely available, but it’s a step toward safer options. Research is also moving toward personalized treatment. Doctors are starting to use stool biomarkers to tell if diarrhea is secretory, osmotic, or inflammatory-and match treatments accordingly. Within five years, we may see blood or stool tests that tell you whether loperamide, bile acid binders, or a low-FODMAP diet will work best for you.When to See a Doctor
See a doctor right away if you have:- Bloody or black stools
- Fever over 38.5°C
- Signs of dehydration (dry mouth, dizziness, little or no urine)
- Weight loss
- Diarrhea lasting more than 14 days
- Severe abdominal pain
Final Takeaway
Acute diarrhea? Focus on hydration. Skip the antibiotics. Use loperamide sparingly and only if you’re miserable and need to get through a day. Chronic diarrhea? This isn’t normal. Don’t just live with it. Get tested. The cause could be treatable-maybe even curable. Loperamide might help, but it’s not the answer. It’s a bridge to finding the real problem. Your gut is talking. Listen before it screams.Is loperamide safe for long-term use?
Loperamide is generally safe for short-term use in acute diarrhea. For chronic conditions like IBS-D, many people use it daily under medical supervision. But long-term use can lead to tolerance-needing higher doses for the same effect. It also carries risks of constipation, dizziness, and, at very high doses, heart rhythm problems. Never exceed 16mg per day without a doctor’s guidance. If you’re taking more than 8mg daily for more than a few weeks, talk to your doctor about alternatives.
Can stress cause chronic diarrhea?
Yes. Stress doesn’t cause diarrhea directly, but it can trigger or worsen conditions like IBS-D. The gut and brain are closely connected through the vagus nerve. When you’re anxious or under pressure, your gut can speed up, leading to urgency and loose stools. Managing stress with therapy, mindfulness, or medication can be just as important as dietary changes.
Should I avoid dairy if I have diarrhea?
During acute diarrhea, many people temporarily lose the enzyme lactase, which breaks down milk sugar. This causes temporary lactose intolerance, making dairy worsen symptoms. Avoid milk, ice cream, and cheese for a few days. Once your gut recovers, you can usually reintroduce dairy. For chronic diarrhea, if you have IBS or celiac disease, dairy may be a trigger-but not always. A low-FODMAP diet can help identify if lactose is the issue.
Is the BRAT diet still recommended?
No. The BRAT diet (bananas, rice, applesauce, toast) was once standard, but experts now say it’s too restrictive and lacks protein and fat needed for recovery. The current advice is to eat a normal, balanced diet as soon as you can tolerate it. Early reintroduction of food helps the gut heal faster. Avoid greasy, spicy, or sugary foods for a day or two, but don’t starve yourself.
Can probiotics cure diarrhea?
Probiotics don’t cure diarrhea, but they can help in specific cases. For antibiotic-associated diarrhea, strains like Lactobacillus rhamnosus GG or Saccharomyces boulardii reduce risk by about 50%. For IBS-D, some people benefit, but results vary. They’re not a magic fix, but they’re safe to try. Look for products with at least 1 billion CFUs and multiple strains.
When should I worry about dehydration?
Dehydration is dangerous, especially in kids and older adults. Signs include dry mouth, sunken eyes, no tears when crying, little or no urine for 8+ hours, dizziness, or extreme fatigue. In children, a sunken soft spot on the head is a red flag. If you’re dizzy, confused, or can’t keep fluids down, seek medical help immediately. Oral rehydration solution is the best treatment-don’t rely on sports drinks or soda.
Can chronic diarrhea lead to other health problems?
Yes. Long-term diarrhea can lead to malnutrition, weight loss, and deficiencies in vitamins like B12, D, and iron. It can also cause skin irritation around the anus and significantly affect mental health-leading to anxiety, depression, or social isolation. That’s why identifying and treating the root cause is critical. Left untreated, chronic diarrhea can be a sign of serious conditions like cancer, Crohn’s, or celiac disease.
Diarrhea might be common, but it’s never just "just a stomach bug." Whether it’s a day or a year, your body is giving you a message. Learn to read it.


Brandon Boyd
January 1, 2026 AT 13:01Just went through a 3-day bug after that food truck sushi. Took 2mg loperamide and was back to normal by noon. Seriously, it’s not magic, but it’s a game-changer when you need to function. Just don’t abuse it-your gut’s got a memory.
Stay hydrated, skip the Gatorade, and make your own ORS with sugar and salt. Works like a charm.
Also, stop eating raw fish from places that don’t have a fridge. Just saying.
Harriet Hollingsworth
January 1, 2026 AT 16:34People are just too lazy to wait for their body to heal. Loperamide is not a cure. It’s a crutch. And now everyone’s popping it like candy. You think your body is a vending machine? Push a button and poof-no diarrhea? No. You’re just hiding the problem. And now we have people taking 100mg a day to get high. That’s not a medical issue. That’s a moral failure.
Deepika D
January 3, 2026 AT 08:00As someone who’s lived with IBS-D for 12 years, I can tell you-loperamide saved my career. I used to miss 2-3 days a week. Now I take 2mg before breakfast and dinner and I’m fine. But here’s the thing: it’s not the drug. It’s the combo. I did the low-FODMAP diet, cut out dairy, started meditation, and yes, I took the meds. It’s not either/or. It’s all of it.
Also, if you think celiac is just "gluten sensitivity," you’re wrong. I was misdiagnosed for 5 years. Blood test + biopsy is non-negotiable. Don’t self-diagnose. Please.
And for the love of all that’s holy, stop telling people to drink apple juice. That’s like pouring gasoline on a fire. Water. Salt. Sugar. That’s it.
Probiotics? I take Align. Not because it’s magic, but because it helps with bloating. It’s not a cure, but it’s a helper. And if you’re on antibiotics, take it 2 hours apart. Timing matters.
Also, stress doesn’t cause IBS, but it turns it into a full-blown nightmare. Therapy helped me more than any pill. Just saying.
Stewart Smith
January 3, 2026 AT 10:05So… loperamide’s basically the opioid of diarrhea? Cool. I’ll just sit here and quietly nod.
Also, why does every medical article feel like it’s written by a guy who’s never had to poop in a public restroom? Just asking.
Retha Dungga
January 3, 2026 AT 20:06life is just a series of loose stools and bad decisions 🤷♀️
but hey at least we got loperamide right? 🙏
my gut is a mood
and today it’s like "nope not today"
so i took 2mg and went to nap 💤
your body talks
you just gotta learn to listen… or just take the pill and pretend you didn’t hear it 😌
Aaron Bales
January 4, 2026 AT 03:50Chronic diarrhea? Get tested. Now. Don’t wait. Bile acid malabsorption after gallbladder removal is super common and treatable. Cholestyramine works. Ask your doctor.
Lawver Stanton
January 4, 2026 AT 13:37Okay so let me get this straight-people are dying from taking too much loperamide because they’re trying to get high? That’s not a medical failure, that’s a cultural collapse. We live in a world where the solution to every problem is a pill. You got heartburn? Take a pill. You’re sad? Take a pill. You got diarrhea? Take a pill. And then you take more pills to fix the side effects of the pills. And then you take pills to fix the side effects of the pills you took to fix the side effects of the original pill. We are not a society. We are a pharmacy with legs.
And don’t even get me started on the BRAT diet. Bananas? Rice? Toast? That’s not food, that’s a punishment. Eat a damn burger if you can tolerate it. Your gut isn’t a kindergarten. It doesn’t need a nap.
Also, I’ve had diarrhea for 3 weeks and I’m still here. So yeah, I’m not going to the doctor. I’m just gonna keep drinking Pedialyte and pretending I’m a warrior.
Who’s with me?
Sara Stinnett
January 6, 2026 AT 07:50Let’s be brutally honest: loperamide is the pharmaceutical equivalent of slapping a Band-Aid on a severed artery. You’re not treating the cause-you’re suppressing the symptom, and in doing so, you’re inviting catastrophe. The FDA’s warning isn’t a suggestion-it’s a funeral notice for the complacent.
And let’s not romanticize "IBS-D" as some quirky, trendy condition. It’s a diagnostic dumpster fire. Half the people who call themselves "IBS" are actually undiagnosed Crohn’s, celiac, or microscopic colitis. And no, your yoga instructor’s turmeric latte isn’t going to fix it.
Also, probiotics? A placebo with a price tag. If you want real results, stop Googling and start getting a colonoscopy. Your dignity is worth more than your pride.
linda permata sari
January 7, 2026 AT 07:50Back home in Indonesia, we use a simple trick: boiled guava leaves. Brew it like tea. It’s natural, cheap, and works better than most pills. My grandma swore by it. And we never had loperamide growing up. Just clean water, rest, and patience.
But I get it-Western medicine loves pills. Still… maybe we’ve forgotten the wisdom of our ancestors?
Not saying ditch the science. Just… maybe mix it with tradition?
Also, no one talks about how embarrassing it is to have to leave a meeting because your gut decides it’s time to revolt. We need more compassion.
And yes, I’ve used loperamide. Once. And I felt like a traitor to my roots. 😅