Digoxin vs Alternative Heart Medications: Pros, Cons, and When to Use
 Oct, 16 2025
Oct, 16 2025
When treating certain heart conditions, digoxin is a cardiac glycoside that helps the heart beat more efficiently and strengthens contraction. It’s been on the market since the 1930s and remains a go‑to option for atrial fibrillation and heart failure. But digoxin isn’t the only game in town. This guide walks through the most common alternatives, weighs their benefits and risks, and helps you decide which drug fits your clinical scenario.
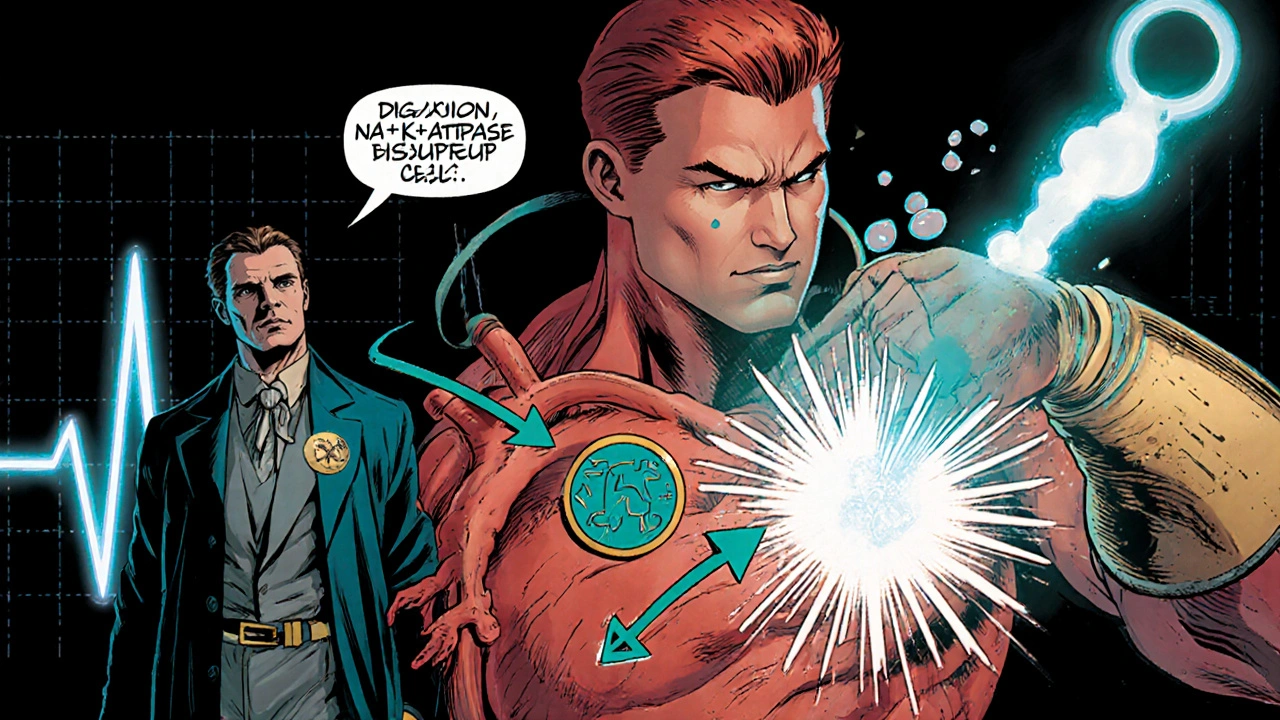
What Digoxin Actually Does
Digoxin inhibits the sodium‑potassium ATPase pump in cardiac cells. The resulting rise in intracellular calcium boosts the force of each heartbeat (positive inotropy) and slows electrical conduction through the atrioventricular node, which can control rapid heart rates.
Typical indications include:
- Atrial fibrillation with rapid ventricular response
- Symptomatic heart failure with reduced ejection fraction
Key advantages are its oral dosing, low cost, and decades of safety data. Common downsides include a narrow therapeutic window, potential for toxic arrhythmias, and the need for regular blood‑level monitoring.
Why Look at Alternatives?
Not every patient tolerates digoxin. Renal impairment, electrolyte imbalances, or interacting medications can push levels into the toxic range. For those cases, clinicians turn to other agents that either support cardiac output differently or target the neurohormonal pathways that drive heart failure.
Top Alternatives Explained
Milrinone - A phosphodiesterase‑3 inhibitor that raises intracellular cAMP, leading to stronger heart muscle contractions and vasodilation. It’s usually given intravenously for acute decompensated heart failure.
Dobutamine is a synthetic catecholamine that stimulates beta‑1 receptors, increasing heart rate and contractility. Like milrinone, it’s delivered IV and reserved for short‑term support.
Carvedilol is a non‑selective beta‑blocker with alpha‑blocking properties. It reduces heart rate, lowers blood pressure, and improves survival in chronic heart failure when titrated slowly.
Lisinopril is an ACE inhibitor that blocks the conversion of angiotensin I to angiotensin II, decreasing afterload and slowing disease progression.
Spironolactone is a potassium‑sparing aldosterone antagonist. It counteracts fluid retention and has proven mortality benefits in patients with reduced ejection fraction.
All these drugs target different parts of the heart‑failure cascade, allowing clinicians to tailor therapy to a patient’s exact needs.

Side‑By‑Side Comparison
| Medication | Mechanism | Typical Use | Advantages | Main Risks |
|---|---|---|---|---|
| Digoxin | Inhibits Na⁺/K⁺‑ATPase → ↑ Ca²⁺ | AFib rate control; chronic HF | Oral, cheap, long history | Narrow therapeutic window, arrhythmia, toxicity |
| Milrinone | Phosphodiesterase‑3 inhibition → ↑ cAMP | Acute decompensated HF (IV) | Increases contractility & vasodilation | Hypotension, arrhythmias, thrombocytopenia |
| Dobutamine | Beta‑1 agonist → ↑ heart rate & contractility | Short‑term HF support (IV) | Rapid onset, easy titration | Myocardial ischemia, tachyarrhythmia |
| Carvedilol | Beta‑blockade + alpha‑blockade | Chronic HF, post‑MI | Improves survival, reduces remodeling | Bradycardia, fatigue, worsened HF early |
| Lisinopril | ACE inhibition → ↓ angiotensin II | Hypertension, chronic HF | Afterload reduction, renal protection | Cough, hyperkalemia, angioedema |
| Spironolactone | Aldosterone antagonism | Chronic HF, resistant hypertension | Reduces fibrosis, improves survival | Hyperkalemia, gynecomastia, renal dysfunction |
How to Choose the Right Medication
Picking the best drug isn’t a one‑size‑fits‑all decision. Consider these three axes:
- Clinical scenario: Acute decompensation often calls for IV agents like milrinone or dobutamine, while stable chronic HF benefits from oral agents such as carvedilol, lisinopril, or spironolactone.
- Patient factors: Renal function, electrolytes, blood pressure, and comorbidities (e.g., asthma, diabetes) shape the safety profile.
- Goal of therapy: Are you aiming to control rate, boost contractility, or modify disease progression?
In many cases, digoxin is added on top of a backbone regimen that already includes a beta‑blocker, an ACE inhibitor, and a mineralocorticoid receptor antagonist. The combination covers rate control, neurohormonal blockade, and contractile support.
Monitoring and Follow‑Up
Regardless of the drug you choose, regular monitoring is vital.
- Digoxin: Check serum levels 6‑8hours after a dose change; aim for 0.5‑2ng/mL. Watch potassium - low levels raise toxicity risk.
- Milrinone/Dobutamine: Monitor blood pressure, heart rate, and urine output continuously while on IV infusion.
- Beta‑blockers: Titrate slowly; watch for worsening HF symptoms in the first weeks.
- ACE inhibitors & spironolactone: Check renal function and potassium at baseline, 1‑2weeks, then quarterly.
Patient education matters, too. Explain signs of digoxin toxicity (nausea, visual changes, palpitations) and when to call the clinic.
Bottom Line
If you need a medication that directly improves heart contractility and slows a rapid heartbeat, digoxin remains a solid, affordable choice. But its narrow safety margin means you must assess kidney function, electrolytes, and potential drug interactions carefully. For acute settings, IV inotropes like milrinone or dobutamine give rapid support. For long‑term disease modification, beta‑blockers, ACE inhibitors, and aldosterone antagonists provide proven mortality benefits. The best regimen often blends a backbone of neurohormonal blockers with a targeted agent such as digoxin or an IV inotrope when needed.
Frequently Asked Questions
What is the therapeutic range for digoxin?
For most adults, the target serum concentration is 0.5‑2ng/mL. Levels above 2ng/mL increase the risk of arrhythmias and other toxic effects.
Can I take digoxin with a beta‑blocker?
Yes, many clinicians combine digoxin with a beta‑blocker like carvedilol to control heart rate and improve contractility. Close monitoring is advised, especially during dose adjustments.
Why might a doctor choose milrinone over digoxin?
Milrinone works via a different pathway (phosphodiesterase‑3 inhibition) and can be given intravenously for rapid effect. It’s preferred in acute decompensated heart failure when oral absorption is unreliable or when the patient has digoxin toxicity.
What are common signs of digoxin toxicity?
Symptoms include nausea, vomiting, loss of appetite, visual disturbances (yellow‑green halos), confusion, and irregular heartbeats. If any appear, seek medical attention promptly.
Is spironolactone appropriate for patients on digoxin?
Spironolactone can be combined with digoxin, but both drugs raise potassium levels. Regular labs are essential to avoid hyperkalemia, which can precipitate serious cardiac events.


Tammie Sinnott
October 17, 2025 AT 13:20Digoxin’s magic lies in its ability to shut down the Na⁺/K⁺‑ATPase pump, which then pumps more calcium into the cardiac cells. That boost in intracellular calcium gives each beat a stronger squeeze, and the slowed AV‑node conduction helps tame rapid atrial fibrillation. It’s cheap, oral, and has been around since the 1930s, so we’ve got a solid safety record to lean on. Just remember the therapeutic window is razor‑thin; you need labs and electrolytes on lock.
Michelle Wigdorovitz
October 18, 2025 AT 17:06When you look at the big picture, it’s all about matching the drug’s route and speed to the patient’s status. IV inotropes like milrinone or dobutamine are lifesavers in an acute decompensation, while oral agents such as carvedilol, lisinopril, or spironolactone shine in chronic management. The art is blending them so you get rate control, neurohormonal blockade, and contractile support without stepping on each other’s toes.
Arianne Gatchalian
October 19, 2025 AT 20:53I always tell patients that the key to staying safe on digoxin is regular blood‑level checks and keeping potassium up. A low‑potassium state can turn a therapeutic dose into a toxic one in no time. Pairing digoxin with a beta‑blocker works great, but you have to watch for bradycardia and adjust doses slowly. Education on the visual changes-yellow‑green halos-is a lifesaver.
Aly Neumeister
October 21, 2025 AT 00:40So, you’ve got digoxin, you’ve got milrinone, you’ve got the whole class-each with its own quirks, each with its own risk profile-choose wisely, watch labs, adjust doses, avoid interactions, and stay vigilant.
joni darmawan
October 22, 2025 AT 04:26From a philosophical standpoint, the selection of a cardiac agent reflects a balance between immediate hemodynamic needs and long‑term disease modification. One must weigh the mechanistic specificity of digoxin against the broader neurohormonal benefits of ACE inhibitors and beta‑blockers, always with an eye toward patient‑centered outcomes.
Richard Gerhart
October 23, 2025 AT 08:13Alright, let’s break this down, step by step, because there’s a lot to chew on when you’re juggling heart meds. First off, digoxin is still a solid option for rate control in atrial fibrillation, especially when you need something cheap and oral. But you can’t ignore its narrow therapeutic index-if the kidneys aren’t clean, you’re walking a tightrope. That’s why I always check creatinine and potassium before even thinking about a dose adjustment.
Now, when a patient comes in with acute decompensated heart failure, IV agents like milrinone or dobutamine become the go‑to weapons. Milrinone gives you both inotropy and vasodilation, which can be a double‑edged sword if blood pressure drops too low. Dobutamine, on the other hand, spikes the heart rate, so you have to watch for ischemia in anyone with CAD.
For chronic management, you want a backbone of neurohormonal blockers: carvedilol, lisinopril, and spironolactone. These have proven mortality benefits, and they work together to blunt the RAAS and sympathetic overdrive. Adding digoxin on top of that can give you that extra contractile push without over‑loading the patient with more drugs.
Don’t forget the monitoring part-digoxin levels every 6‑8 hours after a dose change, potassium checks every few weeks on spironolactone, and blood pressure trends when you’re titrating carvedilol.
Finally, patient education is king. Make sure they know the red flags for digoxin toxicity-nausea, visual halos, confusion-so they can call you before things get scary. In short, the “right” drug depends on the clinical scene, the kidneys, electrolytes, and how many pill bottles the patient can actually manage.
Kim M
October 24, 2025 AT 12:00Big pharma doesn’t want you to know this 🤯
Martin Gilmore
October 25, 2025 AT 15:46Listen up! Digoxin may be cheap, but its toxicity is a silent assassin-watch those serum levels, or you’ll be courting arrhythmias with reckless abandon!
jana caylor
October 26, 2025 AT 18:33Adding to that point, the risk of arrhythmia really spikes when patients are also on diuretics that shift potassium, so double‑check electrolytes before you adjust the dose.
Vijendra Malhotra
October 27, 2025 AT 22:20In many South Asian populations we see a higher prevalence of renal insufficiency, so dose‑reducing digoxin right from the start can prevent a lot of trouble down the line.
Nilesh Barandwal
October 29, 2025 AT 02:06Indeed, careful titration combined with vigilant lab monitoring forms the cornerstone of safe digoxin therapy-precision matters.
Elise Smit
October 30, 2025 AT 05:53From a coaching perspective, think of your medication regimen as a training plan: you need a solid foundation (ACE‑I, beta‑blocker), then layer in specialized work (digoxin or inotropes) when the situation demands it. Consistency and feedback (labs) are key.
Sen Đá
October 31, 2025 AT 09:40It is imperative, therefore, that clinicians adhere to stringent monitoring protocols when prescribing digoxin, especially in the context of comorbid renal disease, to mitigate the inherent risk of toxicity.
LEE DM
November 1, 2025 AT 13:26For patients on multiple agents, a clear medication list and scheduled labs keep everything in sync.
mathokozo mbuzi
November 2, 2025 AT 17:13The decision matrix for heart‑failure therapy must incorporate both acute hemodynamic needs and long‑term neurohormonal modulation, ensuring that each drug’s mechanism aligns with the patient’s clinical trajectory.
Penny X
November 3, 2025 AT 21:00One must not forget the ethical responsibility to prioritize patient safety over convenience; prescribing digoxin without proper monitoring is a breach of the fiduciary duty owed to those we serve.