Dissolution Testing: How the FDA Ensures Generic Drug Quality
 Dec, 11 2025
Dec, 11 2025
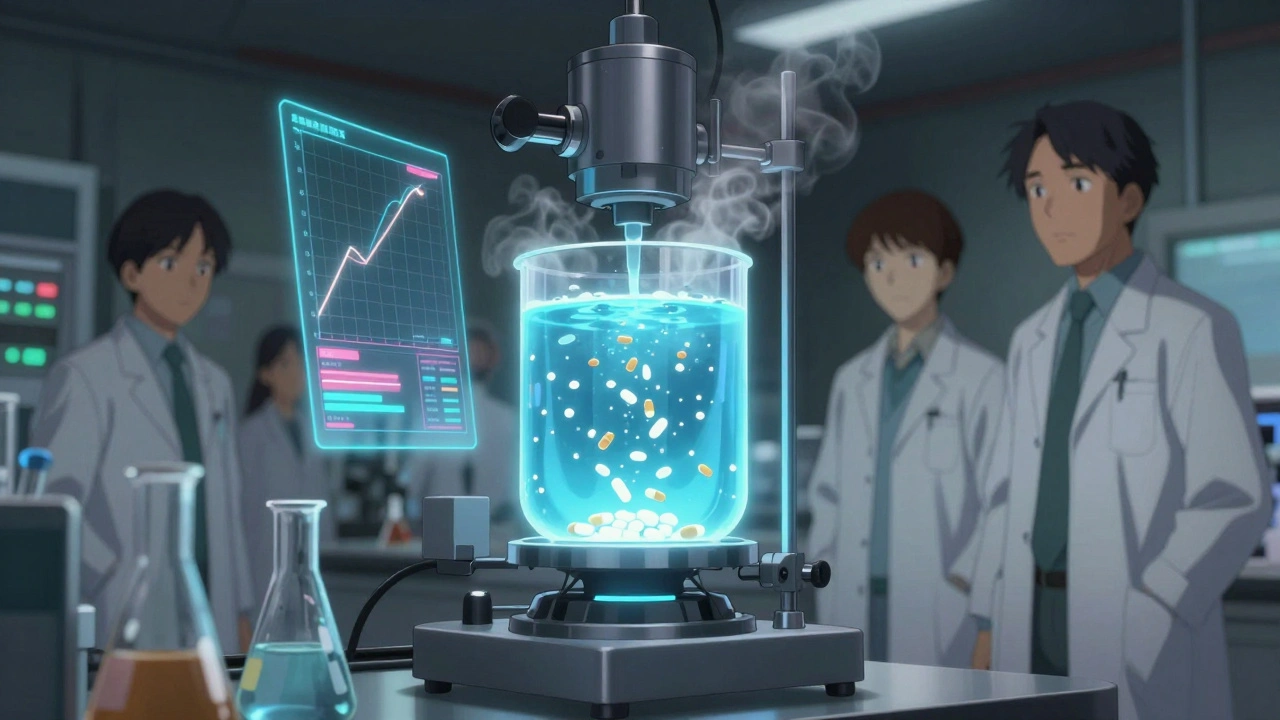
When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But how does the FDA make sure it does? The answer isn’t in human trials-it’s in a lab, with a machine spinning a basket of pills in a beaker of liquid. This is dissolution testing, and it’s the backbone of how the FDA guarantees that generic drugs are safe, effective, and interchangeable.
Why Dissolution Testing Matters
Generic drugs are cheaper because they don’t need to repeat the expensive clinical trials of the original drug. Instead, they must prove they’re bioequivalent-meaning they release the same amount of active ingredient at the same rate in the body. But running human studies for every single generic version? That’s slow, expensive, and unnecessary. That’s where dissolution testing steps in. The FDA uses dissolution testing as a reliable predictor of how a drug will behave inside the body. If a generic pill releases its active ingredient at the same speed and extent as the brand-name version in a controlled lab setting, it’s very likely to perform the same way in patients. This isn’t guesswork-it’s science backed by decades of data and regulatory standards.How the FDA Sets the Rules
The FDA doesn’t just say, “Make it dissolve like the brand.” They lay out exact rules. For every generic drug application (called an ANDA), manufacturers must submit detailed dissolution data across five categories:- How soluble the active ingredient is in different liquids
- Exact test conditions: what machine to use, how fast it spins, what liquid it’s in, how much, and when to take samples
- Proof the test works under small changes-like if the temperature shifts by 1°C
- Validation that the lab can accurately measure how much drug is dissolved
- Proof the test can tell the difference between good and bad formulations
Comparing Profiles: The f2 Factor
It’s not enough to hit a single number. The FDA compares the entire dissolution curve of the generic drug to the brand-name version. They use a statistical tool called the f2 similarity factor. This number, between 0 and 100, tells you how similar the two curves are. An f2 score of 50 or higher means the two products are considered equivalent. A score below 50? The FDA will ask for more data, or reject the application. This isn’t just a formality-it’s a powerful way to catch subtle differences in formulation that could affect how the drug works in the body.
Special Cases: Modified-Release and Low-Solubility Drugs
Not all pills are created equal. Extended-release tablets, like those for high blood pressure or ADHD, are designed to release drug slowly over hours. Dissolving these in just water won’t cut it. The FDA requires testing under multiple pH levels-1.2 (stomach acid), 4.5, and 6.8 (intestinal conditions)-to simulate what happens as the pill moves through the digestive tract. Even worse, some of these drugs are tested with alcohol. Why? Because if a patient takes a slow-release pill with a glass of wine, the alcohol can cause the drug to dump all at once-called “dose dumping.” That’s dangerous. Manufacturers must prove their product won’t do this, even at 40% ethanol concentration. Low-solubility drugs, like many antifungals or cholesterol meds, are another challenge. These drugs don’t dissolve easily, so the test must be sensitive enough to detect tiny changes in formulation. A bad excipient or slightly different particle size could mean the drug doesn’t absorb properly. The FDA demands methods that can spot these differences before the drug ever hits the market.What Happens When the Test Doesn’t Match?
Sometimes, a generic drug passes human bioequivalence studies but fails the dissolution test. The FDA doesn’t automatically reject it. Instead, they may set custom dissolution specifications for that product. This happens when the generic uses a different formulation that still delivers the same results in the body-but behaves differently in the test. The FDA accepts this, but only if the data is rock-solid. It’s rare, but it happens. And it shows the FDA’s approach isn’t rigid-it’s smart. They trust the science, not just the protocol.Why This Saves Time and Money
For BCS Class I drugs-those with high solubility and high permeability-the FDA allows a “biowaiver.” That means no human studies at all. If the generic passes dissolution testing under the standardized conditions, it gets approved. In 2023, about 35% of generic approvals used this shortcut, up from 25% in 2020. That’s thousands of drugs reaching patients faster, without unnecessary trials. This isn’t cutting corners. It’s using science to eliminate waste. Dr. Lawrence Yu, former FDA deputy director, called dissolution testing “a major tool to reduce regulatory burden without sacrificing quality.” And he’s right. Every time a biowaiver is granted, it saves millions in development costs and months of time.
The FDA’s Dissolution Database
Manufacturers don’t have to start from scratch. The FDA maintains a public Dissolution Methods Database with over 2,800 recommended test methods for specific drugs. If your generic matches one of those, you can follow the exact protocol. This cuts development time from 6-12 months down to weeks. But here’s the catch: even if you use a USP method or FDA-recommended method, you still have to prove it works for your specific product. The FDA’s 2023 guidance made that clear. You can’t just copy-paste. You need data. You need validation. You need to show your method is fit for purpose.What Changes After Approval?
Approval isn’t the end. The FDA’s SUPAC-IR guidelines require manufacturers to prove that any change-new factory, different supplier, tweaked excipient-doesn’t alter the dissolution profile. If it does, they must resubmit data. This keeps the quality consistent over time, even as production scales up or moves overseas. This is why you can trust a generic drug bought today will perform the same as one bought a year ago. It’s not luck. It’s regulation.The Bigger Picture
Dissolution testing is more than a lab procedure. It’s a bridge between chemistry and clinical outcomes. It lets regulators approve safe, effective drugs faster, while keeping patients protected. It’s why a $5 generic can be just as reliable as a $50 brand-name pill. The FDA doesn’t just check boxes. They ask: Does this method predict real-world performance? Can it catch a bad batch? Will it work for the next version of this drug? If the answer is yes, the drug gets approved. If not, it’s sent back-with detailed feedback. This system works because it’s grounded in science, not bureaucracy. And it’s why, every day, millions of people around the world take generic drugs with confidence.What is dissolution testing in generic drugs?
Dissolution testing is a lab procedure that measures how quickly a drug releases its active ingredient in a controlled liquid environment. For generic drugs, it’s used to prove they release the drug at the same rate and extent as the brand-name version, ensuring they’ll work the same way in the body without needing human trials.
Why doesn’t the FDA require human studies for every generic drug?
Because dissolution testing is a validated predictor of bioequivalence. For many drugs-especially those that dissolve easily (BCS Class I)-the FDA accepts dissolution data alone as proof of equivalence. This avoids unnecessary, costly, and time-consuming human studies while maintaining safety and effectiveness.
What is the f2 similarity factor?
The f2 similarity factor is a statistical tool used by the FDA to compare the dissolution profiles of a generic drug and its brand-name counterpart. An f2 value of 50 or higher means the two curves are similar enough to be considered equivalent. It’s a key requirement for approval.
Do all generic drugs need the same dissolution test?
No. Dissolution tests are product-specific. Immediate-release pills have different requirements than extended-release tablets. Drugs with low solubility need more complex methods than those that dissolve easily. The FDA tailors the test to the drug’s chemistry and how it’s meant to work in the body.
Can a generic drug be approved even if its dissolution profile is different from the brand?
Yes, but only if human bioequivalence data proves it works the same in the body. The FDA may then set custom dissolution specifications for that generic. This is rare and requires strong evidence, but it shows the FDA prioritizes real-world performance over rigid protocol.
What role does the FDA’s Dissolution Methods Database play?
The database provides over 2,800 pre-approved dissolution methods for specific drugs. Manufacturers can use these as a starting point, saving months of development time. But they still must validate the method for their own product-the FDA won’t accept a copied method without proof it works.
Why is alcohol testing required for some generic drugs?
Some extended-release drugs can release their entire dose too quickly if taken with alcohol-a dangerous condition called dose dumping. To prevent this, manufacturers must test their products in solutions containing up to 40% ethanol to prove they won’t fail under real-world conditions.
How does the FDA ensure quality after a generic drug is approved?
Through SUPAC-IR guidelines, which require manufacturers to prove that any change-like a new factory or ingredient source-doesn’t alter the drug’s dissolution profile. If it does, they must submit new data. This keeps the drug consistent over time, no matter where or how it’s made.


Donna Anderson
December 12, 2025 AT 13:08Rob Purvis
December 12, 2025 AT 14:44sandeep sanigarapu
December 14, 2025 AT 02:35Robert Webb
December 15, 2025 AT 10:24Levi Cooper
December 16, 2025 AT 14:59matthew dendle
December 17, 2025 AT 19:05wendy b
December 18, 2025 AT 23:22Reshma Sinha
December 20, 2025 AT 04:28Laura Weemering
December 20, 2025 AT 13:11Katherine Rodgers
December 21, 2025 AT 02:38Vivian Amadi
December 22, 2025 AT 00:54Jimmy Kärnfeldt
December 22, 2025 AT 04:51john damon
December 22, 2025 AT 13:11Lisa Stringfellow
December 22, 2025 AT 15:45