Gabapentinoids and Opioids Together: What You Need to Know About Respiratory Risks
 Jan, 27 2026
Jan, 27 2026
Respiratory Risk Calculator: Gabapentinoids & Opioids
How This Calculator Works
Based on FDA guidance and clinical evidence, this tool helps you understand your individual risk factors for respiratory depression when taking gabapentinoids (gabapentin, pregabalin) with opioids. It uses 12 key factors to estimate risk levels and provide safety recommendations.
Enter your clinical details to assess your respiratory risk:
Combining gabapentinoids like gabapentin or pregabalin with opioids might seem like a smart way to manage pain-less opioid use, better control. But what if this combo is quietly putting your breathing at risk? It’s not just a theory. Since 2019, the FDA has required strong warnings on these drugs because real people have stopped breathing after taking them together. This isn’t rare. It’s underreported, misunderstood, and often missed until it’s too late.
Why Doctors Used to Prescribe This Combo
For years, gabapentinoids were seen as helpful sidekicks to opioids. After surgery, patients got gabapentin or pregabalin to reduce nerve pain. The idea was simple: lower the opioid dose by 20-30%, cut down on side effects like nausea and constipation, and still keep pain under control. Many hospitals made this a standard protocol. Studies showed it worked-on paper. Pain scores dropped. Opioid use decreased. Everyone breathed easier-until they didn’t.The Hidden Danger: How These Drugs Team Up Against Your Breathing
Gabapentinoids don’t just block pain signals. They slow down the part of your brain that tells your lungs when to breathe. Opioids do the same thing. When you take both, the effect isn’t just added-it’s multiplied. Your body’s natural alarm system for low oxygen gets dulled. You might not even feel like you’re struggling to breathe until it’s too late. Here’s what’s happening inside your body: Opioids slow down your gut. That means gabapentinoids sit longer in your intestines and get absorbed more fully-up to 44% more than if taken alone. That extra drug hits your brain harder. At the same time, gabapentinoids make your brain less sensitive to carbon dioxide. Normally, when CO2 builds up, your body kicks in to breathe faster. With this combo, that reflex weakens. The result? Slower, shallower breaths. Silent, deadly.Who’s at Highest Risk?
Not everyone who takes this combo will have problems. But some people are sitting on a ticking clock:- People over 65-their bodies clear drugs slower, and their breathing control is naturally weaker.
- Those with sleep apnea or COPD-their lungs are already working hard. Adding these drugs pushes them past their limit.
- People with kidney problems-both gabapentin and pregabalin are cleared by the kidneys. If your kidneys aren’t working well, the drugs build up.
- Those on high opioid doses-the higher the opioid, the greater the danger when gabapentinoids are added.
- Patients in the first 24-72 hours after surgery-this is when most cases of respiratory depression occur.
A 2022 UK study found people on both drugs were 38% more likely to die from an accidental overdose than those on opioids alone. Another study showed that in patients with sleep apnea, the risk of needing emergency breathing support jumped by 40% after hospitals stopped using gabapentinoids in opioid-treated patients.
The Numbers Don’t Lie-But They’re Misunderstood
Some studies say the risk is “low.” That’s true-if you look at the whole population. Out of 16,000 patients, maybe only a few had serious breathing problems. But that’s not how risk works in real life. You’re not a statistic. You’re the person with sleep apnea. You’re the 70-year-old with kidney disease. You’re the one getting 300mg of gabapentin and 20mg of morphine after a hip replacement. The problem isn’t the average risk. It’s the unpredictable risk. One person might take the same dose and feel fine. Another might slip into respiratory arrest without warning. That’s why experts say: don’t rely on population data to decide what’s safe for you.What the Experts Are Saying Now
The American Geriatrics Society, the FDA, and the UK’s Medicines and Healthcare products Regulatory Agency all agree: avoid this combo if you can. The 2019 Beers Criteria-used by doctors nationwide to guide safe prescribing-explicitly says not to use gabapentinoids with opioids in older adults. Dr. Janet Woodcock, former FDA deputy commissioner, said it plainly: “There are serious consequences of this co-use, including respiratory depression and increased risk of opioid overdose death.” Even pain specialists who once pushed this combo are changing their minds. One anesthesiologist on Reddit shared a case where a 58-year-old man with mild COPD needed naloxone after just 300mg of gabapentin and 20mg of morphine. He was supposed to be low-risk. He wasn’t.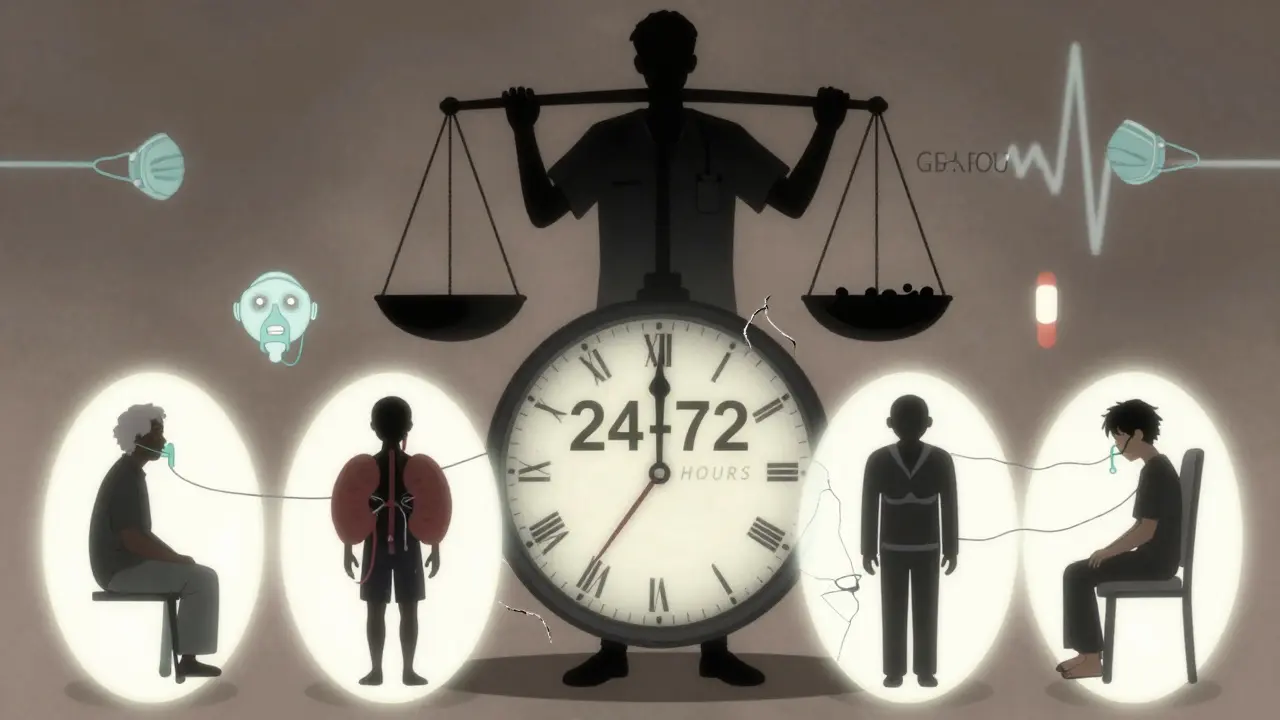
What Should You Do If You’re on This Combo?
If you’re currently taking gabapentin or pregabalin with an opioid, don’t stop suddenly. Talk to your doctor. Ask these questions:- Is this combo still necessary? Could I switch to non-addictive pain relievers like acetaminophen or NSAIDs?
- Am I on the lowest possible dose of both drugs?
- Do I have any risk factors-age, sleep apnea, kidney issues, COPD?
- Have I been monitored for breathing changes, especially after surgery or dose changes?
If you’re in the hospital or recovering from surgery, ask for pulse oximetry (to check oxygen levels) and capnography (to measure CO2). These tools catch breathing problems before you even feel them. Many hospitals now use them for high-risk patients-but not all. Push for it.
What’s Changing in 2026?
Prescriptions for gabapentinoids have dropped 12% since 2018, and co-prescribing with opioids is falling faster. The FDA required drugmakers to run new clinical trials on this exact interaction. Results are due in 2025. Meanwhile, the CDC updated its opioid guidelines in 2022 to say: “Avoid gabapentinoids with opioids when possible.” A new risk calculator is coming in mid-2024. It will use 12 factors-age, kidney function, opioid dose, BMI, sleep apnea history-to predict who’s most likely to have breathing trouble. Early tests show it’s 87% accurate at spotting high-risk patients.What’s the Bottom Line?
Gabapentinoids aren’t evil. They help people with nerve pain, seizures, and anxiety. Opioids aren’t evil either-they save lives in acute pain. But together, they create a silent, invisible threat. The risk isn’t big for everyone. But for some, it’s deadly.Don’t assume it’s safe because your doctor prescribed it. Don’t assume it’s rare because a study says so. Ask. Monitor. Push for safer alternatives. Your breathing is worth it.
Can gabapentin or pregabalin cause breathing problems on their own?
Yes. While the risk is much higher when combined with opioids, gabapentinoids alone can cause respiratory depression, especially in older adults, people with kidney disease, or those taking high doses. The UK’s MHRA confirmed in 2022 that gabapentin has been linked to rare but severe cases of breathing difficulty even without opioids.
Is it safe to take gabapentinoids with opioids if I’m on a low dose?
Low doses reduce risk but don’t eliminate it. Even 300mg of gabapentin with 10mg of oxycodone has caused respiratory depression in vulnerable patients. Dose isn’t the only factor-your age, lung health, kidney function, and sleep apnea status matter more. If you have any of these risk factors, avoid the combo even at low doses.
What should I do if I feel unusually sleepy or my breathing feels shallow?
Don’t wait. If you’re taking this combo and feel drowsier than normal, your breathing feels slow or shallow, or you’re having trouble staying awake, seek medical help immediately. Call 911 or go to the ER. This is a medical emergency. Naloxone can reverse opioid effects but won’t help with gabapentinoid-induced respiratory depression. You need oxygen and monitoring.
Are there safer alternatives to gabapentinoids for nerve pain with opioids?
Yes. For nerve pain, consider duloxetine (Cymbalta), amitriptyline (a low-dose tricyclic antidepressant), or topical lidocaine patches. For general pain, acetaminophen and NSAIDs like ibuprofen are safer when used appropriately. Physical therapy, nerve blocks, and cognitive behavioral therapy can also reduce reliance on both opioids and gabapentinoids.
Why haven’t more people heard about this risk?
Because the risk was hidden behind the success of reduced opioid use. Doctors focused on the benefit-less morphine-without seeing the hidden cost. Also, respiratory depression from this combo often happens quietly, without obvious signs like vomiting or pinpoint pupils. It doesn’t make headlines. But it’s in the death certificates. And now, the data is clear.


matthew martin
January 28, 2026 AT 19:25Been on gabapentin for years after a car wreck. Never thought about how it might be quietly killing my breath until I read this. My doc just shrugged when I asked about the combo with oxycodone. Now I’m scared to even take my nightly dose. Guess I’m scheduling a talk with my pain specialist tomorrow.
Wish more doctors would stop treating these drugs like harmless candy.
Robert Cardoso
January 29, 2026 AT 12:40Let’s be real-this isn’t new. The FDA warning in 2019 was a joke. It took three years and dozens of dead elderly patients before they bothered to slap a label on it. Meanwhile, hospitals still use this combo like it’s a fucking recipe for pain management. The system doesn’t care about you. It cares about discharge times and billing codes.
Stop blaming doctors. Blame the profit-driven machine that rewards volume over vigilance.
jonathan soba
January 31, 2026 AT 02:19Interesting how the risk is ‘low’ in population studies but catastrophic in practice. That’s the exact flaw in evidence-based medicine-it ignores heterogeneity. A 38% increase in mortality sounds abstract until you’re the 38%.
Also worth noting: gabapentinoids are often prescribed for off-label anxiety or insomnia, not neuropathic pain. That’s where the real abuse lies. Doctors think it’s safe because it’s not a controlled substance. It’s not. But it’s still dangerous.
doug b
January 31, 2026 AT 12:28Hey-if you’re on this combo and you’re feeling sleepy or your breathing feels off, don’t wait. Call your doctor. Or better yet, go to urgent care. I’ve seen too many people wait until they’re blue in the face. It’s not dramatic. It’s quiet. And that’s why it kills.
You’re not overreacting. You’re being smart.
Katie Mccreary
February 2, 2026 AT 12:20My grandma died from this. No one told us. She was on 300mg gabapentin and 15mg oxycodone after her hip surgery. They said she ‘just stopped breathing.’ No warning. No monitoring. No nothing.
Now I’m the family enforcer. No more gabapentin. Ever.
Mel MJPS
February 4, 2026 AT 04:37Thank you for writing this. I’ve been terrified to ask my doctor about my meds because I don’t want to sound like a hypochondriac. But now I know I’m not. This is real. I’m printing this out and taking it to my appointment next week.
You’re not alone if you’re scared. I’m right there with you.
Irebami Soyinka
February 6, 2026 AT 02:28Of course this happens. Western medicine treats pain like a math problem-add drug A, subtract pain. But the body isn’t a spreadsheet. It’s a living thing with limits. We’ve been poisoning ourselves with pills for decades and calling it ‘progress.’
Meanwhile, in Nigeria, we use ginger, heat, and prayer. No one dies from ‘natural pain relief.’ Just saying.
Kathy Scaman
February 7, 2026 AT 11:22I’m a nurse. We stopped giving gabapentin with opioids in our ICU last year. No more respiratory arrests. No more code blues from ‘unexplained’ sedation.
It’s not that hard to change. We just had to stop being lazy and start thinking.
Mindee Coulter
February 8, 2026 AT 06:58My dad was on this combo for years after his back surgery. He never complained. He just got quieter. We thought he was aging. Turns out he was slowly suffocating. He’s okay now-switched to lidocaine patches and physical therapy. But I wish we’d known sooner.
Ask questions. Even if it feels awkward.
Phil Davis
February 9, 2026 AT 12:20So the solution is to avoid gabapentinoids with opioids… unless you’re a 70-year-old with kidney disease and sleep apnea. Then the solution is to avoid gabapentinoids with opioids. Wow. Groundbreaking.
Meanwhile, the pharmaceutical companies are probably laughing all the way to the bank while we’re all just now catching up to what we should’ve known in 2015.
Bryan Fracchia
February 9, 2026 AT 15:57There’s a deeper truth here: we’ve outsourced our pain management to pills because we’re scared of discomfort. We don’t want to sit with the ache. We don’t want to do the hard work of therapy or movement or mindfulness.
Gabapentinoids and opioids are the chemical version of ignoring your problems. They don’t fix anything. They just make you forget you’re hurting.
Maybe the real solution isn’t a new drug-it’s a new relationship with pain.
Jeffrey Carroll
February 11, 2026 AT 04:53As a retired physician, I’ve seen this pattern repeat for over two decades. The medical community loves a ‘win’-lower opioid use, lower addiction rates. But we ignored the collateral damage. Respiratory depression isn’t sexy. It doesn’t make for a good case study. It just kills people quietly.
I’m glad the guidelines are changing. I just wish they’d changed before the first death.