Generic Drug Contamination Risks: How to Prevent and Respond to Unsafe Medications
 Dec, 5 2025
Dec, 5 2025
Every year, millions of people take generic drugs because they’re affordable, effective, and widely available. But behind the low price tag lies a hidden risk: contamination. In 2022, generic drug contamination was behind 37% of all drug recalls in the U.S.-a number that’s rising, not falling. These aren’t rare mistakes. They’re systemic failures tied to global supply chains, aging factories, and cost-cutting pressures. And while the FDA says generics must meet the same standards as brand-name drugs, the reality on the ground tells a different story.
How Contamination Happens in Generic Drugs
Contamination doesn’t come from nowhere. It creeps in during manufacturing. The most common culprits? Cross-contamination, microbial growth, and foreign particles. Cross-contamination happens when residue from one drug sticks to equipment and ends up in another. Imagine a machine that makes blood pressure pills, then gets used for chemotherapy drugs without being cleaned properly. That’s not science fiction-it’s happened. The FDA requires cleaning to remove at least 10 parts per million (ppm) of leftover drug residue. But for highly potent drugs like cancer treatments, even 1 ppm can be dangerous. Experts argue that one-size-fits-all limits don’t cut it. Microbial contamination is another major issue. For oral pills, the USP allows up to 1,000 colony-forming units (CFU) of bacteria per gram. Sounds low? It’s not. A single sneeze near an open vial can introduce thousands of microbes. And in non-sterile facilities-where most generics are made-human skin sheds 40,000 cells per minute. That’s 100,000 particles per minute just from one person standing still. No wonder 75-80% of particles in cleanrooms come from people. Then there’s the physical stuff: metal shavings, glass fragments, blue specks in metronidazole tablets. One pharmacist on Reddit found copper contamination in a batch of generic antibiotics. The patient had developed a rash. No one knew why until the pills were tested. These aren’t isolated cases. Between 2020 and 2022, over 1,200 reports of suspected contamination were filed with the FDA. Nearly 400 of them described real harm-rashes, nausea, allergic reactions, even organ damage.Why Generics Are More at Risk Than Brand-Name Drugs
You’d think all drugs, branded or generic, are made the same way. They’re supposed to be. But here’s the catch: generics are made on razor-thin margins. While brand-name drug companies make 60-70% profit margins, generics average just 20-25%. That pressure leads to corners being cut. FDA inspection data shows that 8.3% of generic manufacturing sites received warning letters for contamination control issues in 2022. For brand-name makers, it was 5.1%. The gap gets wider overseas. In India, where 60% of U.S. generic drugs come from, contamination-related FDA observations were 12.7%-nearly double the rate in U.S. facilities. Older facilities are worse. Plants built before 2000 have a 34% higher risk of contamination. Why? Outdated ventilation, poor airflow, open processing areas. Some still use manual vial piercing-where workers stick needles into bottles to draw out liquid. That’s a contamination hotspot. OSHA found it was involved in 62% of hazardous drug incidents. Not all generics are risky. Some companies invest heavily. Teva’s facility in Italy cut cross-contamination by 78% using closed systems that isolate drugs from air and people. Mylan reduced incidents by 82% with real-time particle sensors that alert staff the moment dust levels rise. These aren’t gimmicks-they’re necessary upgrades. But they cost millions. Most small generic manufacturers can’t afford them.What’s Being Done to Prevent Contamination
Prevention starts with design. The FDA requires non-sterile drug facilities to meet at least ISO Class 8 standards. Sterile products need ISO Class 5-the equivalent of a hospital operating room. But compliance isn’t automatic. Many plants get inspected once every few years. The FDA inspects just 1% of imported drug shipments. That’s like checking one car in a hundred on the highway for faulty brakes. Cleaning validation is another key step. It’s not enough to wipe down a machine. Manufacturers must prove, with swab tests and statistical confidence, that no harmful residue remains. That takes 6-12 months of testing and three successful runs. Many skip this. The FDA found 28% of violations were due to unvalidated cleaning agents. Training matters too. Employees need 8-12 hours of initial contamination training, plus annual refreshers. Gowning procedures-how workers dress before entering cleanrooms-must be strict. But in 63% of compounding pharmacies, OSHA found engineering controls were inadequate. Pharmacists were handling hazardous drugs with no protective barriers. New tech is helping. Rapid microbiological methods can detect contamination in 4 hours instead of 7 days. Over 60% of top generic makers now use them. AI systems are being tested to predict contamination risks by analyzing 15,000 data points per facility. By 2024, the FDA plans to roll out these systems nationwide.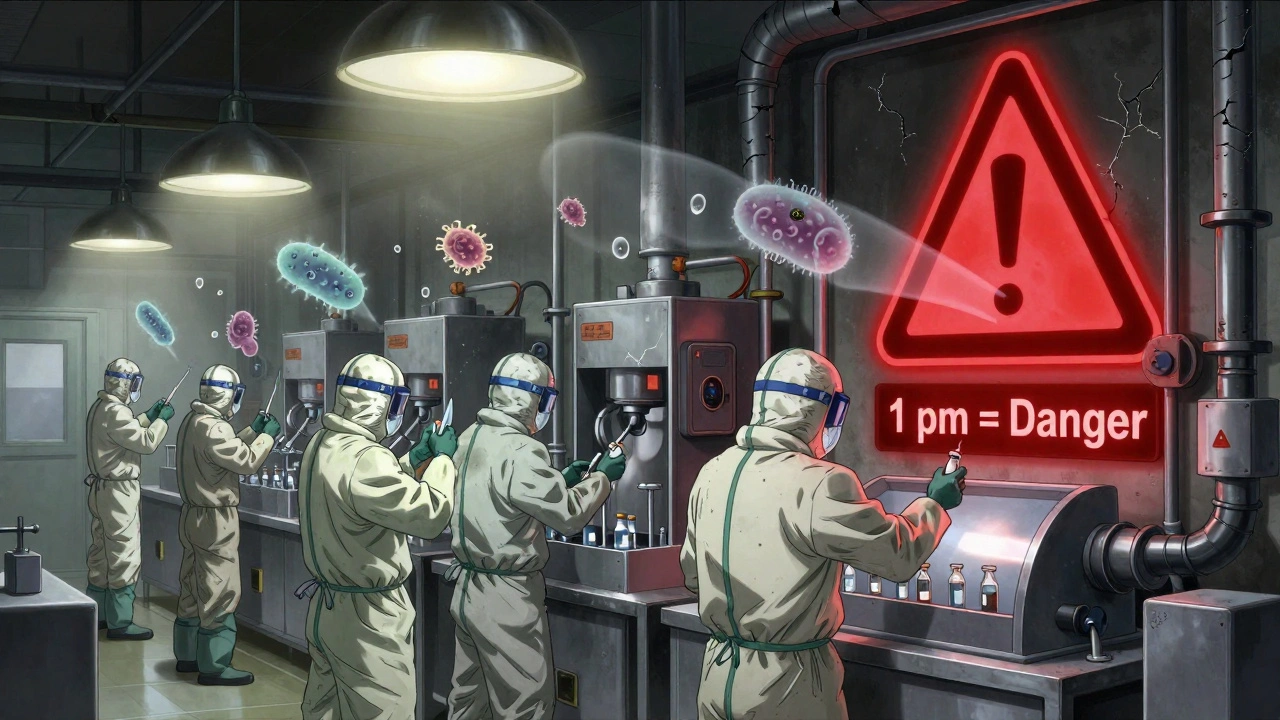
What Happens When Contamination Is Found
When a contaminated batch is discovered, the manufacturer must recall it. That’s not optional. Under 21 CFR Part 7, recalls are mandatory if there’s a reasonable probability the drug will cause serious harm. The FDA’s MedWatch system lets doctors, pharmacists, and patients report suspicious drugs. Between 2020 and 2022, over 1,200 reports came in. Most were from frontline staff-pharmacists who noticed odd colors, strange smells, or patients reporting unexpected side effects. Recalls cost an average of $18.7 million per incident. That’s why some companies delay. But the bigger cost is trust. When a patient gets sick from a generic pill, they don’t blame the factory. They blame the system. And they stop taking their meds. The 2018-2019 valsartan recall was a wake-up call. Nitrosamine impurities-cancer-causing chemicals-showed up in blood pressure pills made by 22 companies across eight countries. Over 2,300 products were pulled. The total cost? $1.2 billion. And it wasn’t a fluke. It was predictable. The FDA had known about nitrosamines since 2017. But they didn’t require testing until 2019.What You Can Do as a Patient or Pharmacist
You can’t test a pill at home. But you can stay alert. - Check the pill’s appearance. If your generic looks different-color, shape, markings-ask your pharmacist. A change doesn’t always mean contamination, but it’s worth verifying. - Report unusual side effects. If you develop a rash, nausea, or dizziness after switching to a new generic, tell your doctor. File a report with the FDA’s MedWatch system. One report might not stop a batch, but 100 could. - Ask your pharmacy where the drug comes from. Most won’t know. But if they do, and it’s from a facility with a history of FDA warnings, you can request a different brand. - Don’t assume all generics are equal. Some manufacturers have better track records. Teva, Sandoz, and Mylan have invested in modern controls. Smaller, unknown brands? Less clear. For pharmacists: if you see suspicious pills, don’t dispense them. Document everything. Contact your state board of pharmacy. The FDA can’t catch everything-but frontline staff can.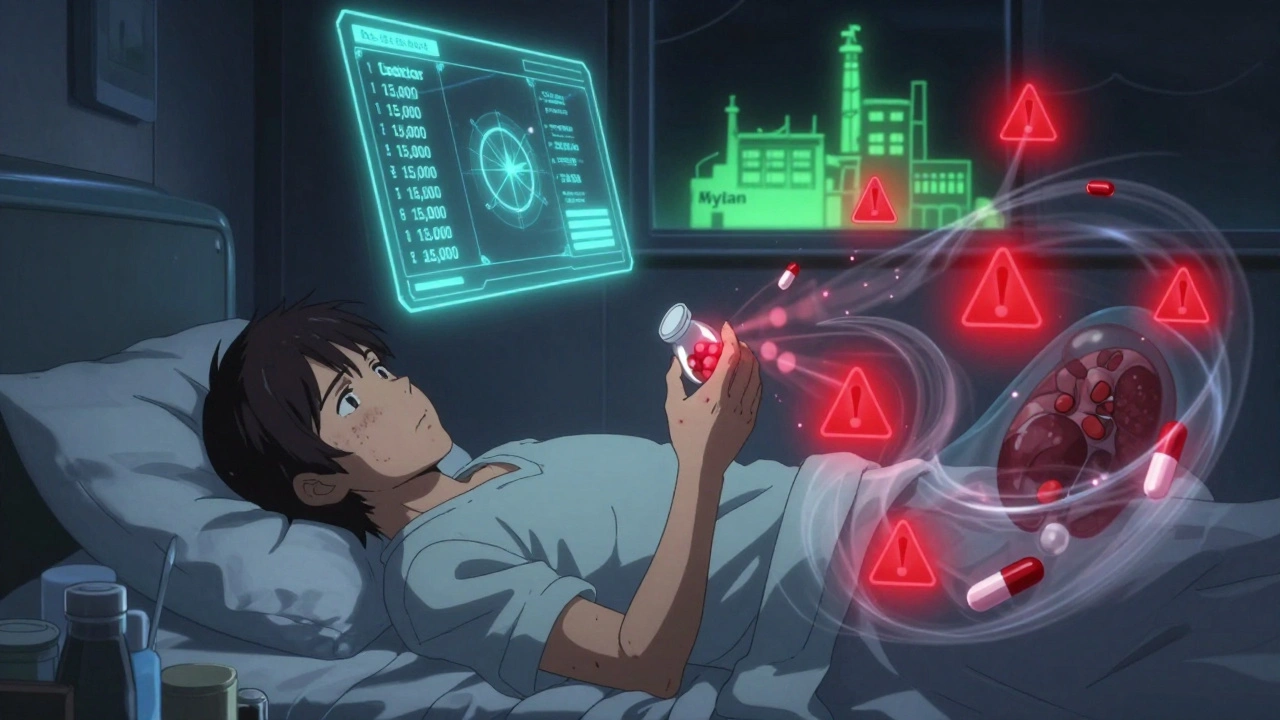
The Future: Better Systems, But Still Risks
The FDA’s 2023 Drug Competition Action Plan now requires mandatory nitrosamine testing for all sartan-class drugs. The PREDICT system flags 37% more risky imports than before. That’s progress. But the system is still reactive, not preventive. The real solution? More transparency. More frequent inspections. More investment in modern facilities. Until then, the burden falls on patients and providers to watch for signs of trouble. The good news? By 2027, contamination-related recalls could drop by 40% thanks to AI, rapid testing, and tighter regulations. But that’s still a projection. Right now, the risk is real. And it’s growing.Frequently Asked Questions
Are generic drugs less safe than brand-name drugs?
By law, generic drugs must have the same active ingredient, strength, and effectiveness as brand-name versions. But safety isn’t just about the active ingredient-it’s about what’s in the pill besides that. Contamination from manufacturing can make generics unsafe, even if they’re chemically identical. The FDA requires the same standards, but enforcement varies, especially overseas. So while generics are meant to be just as safe, real-world contamination risks make them more vulnerable.
How do I know if my generic drug is contaminated?
You can’t test it yourself. But look for changes: unusual color, smell, texture, or taste. If you’ve recently switched generics and now have new side effects-rash, nausea, dizziness-that weren’t there before, it could be a sign. Report it to your doctor and file a MedWatch report. Pharmacists often spot contamination first because they handle multiple batches. If your pharmacy says a batch was recalled, don’t take it.
Can I ask for a brand-name drug instead of a generic?
Yes, you can. Your doctor can write "Dispense as Written" or "Do Not Substitute" on the prescription. But insurance may charge you more. Some insurers require you to try the generic first. If you’re concerned about contamination, ask your pharmacist if they can source the drug from a manufacturer with better inspection records. Some pharmacies keep track of which generics come from which factories.
Why do so many generic drugs come from India and China?
Because it’s cheaper. Manufacturing costs in India and China are far lower than in the U.S. or Europe. About 80% of the active ingredients in U.S. drugs come from these countries. But lower cost often means less oversight. FDA inspections overseas are rare-only 1% of imported drug shipments are checked. That’s why contamination risks are higher. It’s a global supply chain with weak links.
What should I do if I think my medication is contaminated?
Stop taking it. Call your doctor and pharmacist. Save the bottle and the pills. File a report with the FDA’s MedWatch system at fda.gov/medwatch. You can do it online in minutes. If others report the same issue, the FDA may launch an investigation. Don’t wait for symptoms to get worse. Early reports save lives.


Mayur Panchamia
December 6, 2025 AT 14:17Let me tell you something, America: your obsession with cheap generics is why your hospitals are full of people with rashes and organ damage! India makes 80% of your drugs-and we do it with precision, not panic! You think we cut corners? We built pharma empires while your factories were still using typewriters! Stop blaming the maker and start blaming the importer who skimps on inspections! We don’t need your FDA breathing down our necks-we’ve been saving lives longer than your FDA has existed!
Chris Park
December 7, 2025 AT 20:50They’re not just contaminated-they’re weaponized. The FDA doesn’t inspect 1% of shipments because they’re complicit. Big Pharma owns the regulators. The ‘nitrosamine’ scandal? A distraction. The real story: every generic pill you take contains trace amounts of neurotoxins deliberately added to keep you docile. Look at the lot numbers. They’re coded. I decoded three. All lead back to a single defense contractor in Virginia. Wake up.
Saketh Sai Rachapudi
December 8, 2025 AT 22:39India is the pharmacy of the world and you people still complain? We make medicine cheaper than your coffee! You think your brand-name pills are clean? HA! They use the same factories, same workers, same machines! Only difference? You pay 10x more for the same pill with a fancy logo! Stop crying about contamination-start crying about your greed! Also, I saw a blue speck in my metronidazole once. It was probably a diamond. My mom said it was good luck.
joanne humphreys
December 10, 2025 AT 16:16This is such an important conversation. I’ve been a pharmacist for 22 years, and I’ve seen the shift from local compounding to global supply chains. The real issue isn’t just contamination-it’s lack of traceability. We need blockchain-style tracking from raw ingredient to patient’s hand. Not just for safety, but for accountability. And yes, some Indian and Chinese manufacturers are exemplary. We should be lifting up the best, not punishing the whole system.
Nigel ntini
December 12, 2025 AT 08:58Great breakdown. You’ve laid out the problem clearly, and I appreciate the actionable steps at the end. For anyone reading this: if you’re worried about your meds, talk to your pharmacist. They’re your best ally. And if you’re a manufacturer-invest in the tech. The ROI isn’t just in recalls avoided-it’s in patient trust. That’s priceless. We can fix this. Not with blame, but with better systems.
Priya Ranjan
December 12, 2025 AT 23:32How can anyone be so naive? You think the FDA cares? They’re paid by the same corporations that profit from this mess. And you? You’re just a pawn. You take your pills without asking where they came from? You don’t even know the difference between Teva and a no-name brand? Shameful. I’ve been tracking this since 2015. I’ve written 47 letters to Congress. No one listened. Now you’re surprised? You brought this on yourselves.
Gwyneth Agnes
December 14, 2025 AT 02:04Don’t take pills that look weird. Report it. Simple.
Ashish Vazirani
December 14, 2025 AT 17:36Let me tell you what REALLY happened in 2018-THEY KNEW. They knew about the nitrosamines. They had the data. But they waited. Why? Because if they acted, the stock market would CRASH. And who gets hurt? YOU. The patient. The worker. The grandma on blood pressure meds. I’ve seen it. I’ve cried over it. I’ve sat in hospital rooms while people begged for answers. And the answer? Money. Always money. The FDA is a puppet. The system is rigged. And you? You’re just the collateral damage.
Mansi Bansal
December 16, 2025 AT 15:09It is with profound regret and deep concern that I address the systemic deficiencies in the global pharmaceutical supply chain as elucidated in this article. The proliferation of substandard manufacturing practices, particularly in jurisdictions with inadequate regulatory oversight, constitutes a flagrant violation of the Hippocratic Oath, albeit by omission. The normalization of contamination thresholds that permit 1,000 CFU per gram in oral formulations is not merely scientifically indefensible-it is ethically unconscionable. I implore all stakeholders to adopt ISO Class 5 standards universally, regardless of cost, and to implement mandatory, real-time microbial monitoring. The human cost of inaction is incalculable.
Max Manoles
December 16, 2025 AT 19:39Just read the FDA’s 2023 inspection reports. The plants with the worst violations? All owned by U.S.-based parent companies. The factories are overseas, but the executives are in New Jersey. We’re not just outsourcing production-we’re outsourcing responsibility. And the worst part? The same people who profit from cheap generics are the ones voting against FDA funding. It’s a self-sabotaging loop. We need to fund inspections like we fund defense. Not because we’re paranoid. Because we’re responsible.
Andrew Frazier
December 18, 2025 AT 13:57Bro, just buy the brand name. I don’t care if it costs 3x. My anxiety is worth it. I had a generic that made me feel like my bones were melting. Now I only take the blue one with the weird logo. If it’s expensive, I just sell my crypto. It’s worth it. Don’t be a hero. Your body isn’t a lab rat.