Head Injury While on Blood Thinners: When to Get Imaging
 Dec, 3 2025
Dec, 3 2025
Head Injury Risk Calculator
This tool helps assess your risk of serious brain injury if you're on blood thinners and have hit your head. Based on guidelines from the American College of Emergency Physicians.
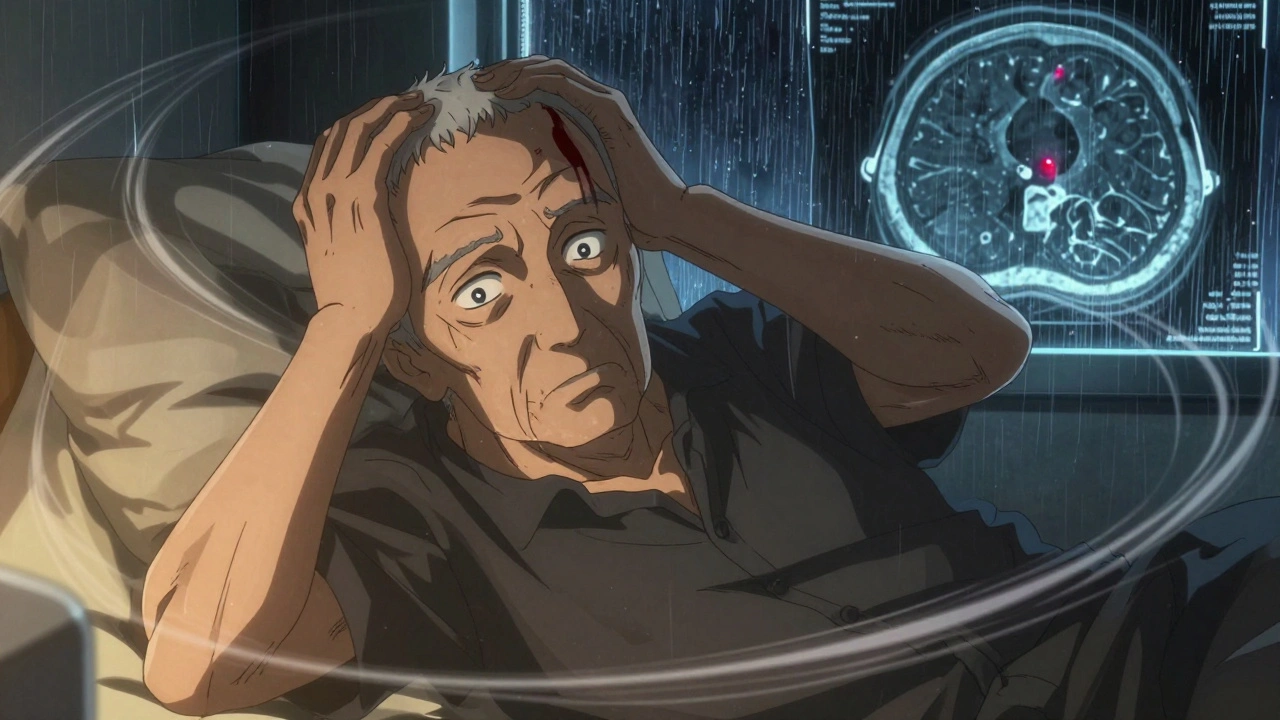
If you're on blood thinners and you hit your head-even if it feels like a minor bump-you can't afford to wait and see. The risk of internal bleeding in the brain is real, and it doesn't always show up right away. What feels like a simple fall or a bump on the head could turn into a life-threatening situation hours or even days later. That’s why imaging isn’t optional in these cases. It’s the first and most critical step.
Why Even a Small Head Injury Is Dangerous on Blood Thinners
People on anticoagulants like warfarin, rivaroxaban, apixaban, or aspirin have blood that doesn’t clot as easily. That’s good for preventing strokes or clots in the legs, but it’s dangerous when trauma happens. A small bleed inside the skull can grow slowly, with no obvious symptoms at first. By the time someone feels dizzy, confused, or vomits, it might already be too late.
Studies show that people on blood thinners are 2 to 3 times more likely to have a serious brain bleed after even a minor head injury than those not on these medications. The risk doesn’t disappear just because you didn’t lose consciousness or feel dizzy right away. In fact, many of the worst cases happen in people who seemed fine at first.
One study found that 0.5% to 1% of anticoagulated patients with a normal initial CT scan still developed a delayed bleed within days. That’s not rare. That’s one in every 100 to 200 people. And if you’re 65 or older, your risk goes up even more.
When Imaging Is Non-Negotiable
Guidelines from the American College of Emergency Physicians (ACEP) and state health departments like Washington State agree: if you’re on blood thinners and you’ve had a head injury, get a CT scan-right away.
You don’t need to wait for symptoms. You don’t need to be told you’re at risk. If any of these happened, get scanned:
- You lost consciousness-even for a few seconds
- You have confusion, trouble remembering things, or feel "foggy"
- You fell from a height (even just one level, like down stairs)
- You were hit directly on the head or neck
- You have a visible bump, cut, or bruise on your head
- You’re 65 or older
- You’re vomiting more than once
- You have trouble walking, speaking, or seeing clearly
These aren’t "maybe" signs. They’re triggers. Emergency rooms across the U.S. and Australia follow this protocol. If you’re on blood thinners and you’ve had any of these, you’ll be fast-tracked to the CT scanner. No waiting. No "let’s monitor you first."
What the CT Scan Looks For
The scan isn’t just a quick check. It’s a detailed look at the inside of your skull. The machine uses very thin slices-between 0.5 mm and 1.25 mm-to catch tiny cracks in the skull or small bleeds that might be missed with standard imaging.
Doctors are looking for:
- Subdural hematoma (blood between the brain and its outer lining)
- Epidural hematoma (blood between the skull and the brain’s outer covering)
- Intracerebral hemorrhage (bleeding inside the brain tissue)
- Skull fractures
Even a tiny amount of blood can be dangerous on blood thinners because it keeps spreading. A 2 mm bleed today could become a 20 mm bleed by tomorrow. That’s why timing matters.
What Happens After the Scan
If the CT scan shows no bleeding, you might still need to stay under observation. Some hospitals send you home after 6 hours if you’re stable, your INR is under 3.5 (if you’re on warfarin), and you have no other injuries. Others keep you overnight.
Why the difference? Because research shows delayed bleeds can happen up to 72 hours after the injury. One patient in a Texas hospital had a normal CT, stopped his rivaroxaban, and had a stroke three days later. That’s the catch: stopping your blood thinner can be just as dangerous as not treating the bleed.
So here’s the balance: you need to watch for new symptoms-worsening headache, confusion, weakness on one side, slurred speech, or seizures-while still staying on your medication unless a doctor tells you otherwise. Never stop your blood thinner on your own.

What You Shouldn’t Do
There are common mistakes people make after a head injury on blood thinners:
- Waiting to see if symptoms get worse
- Assuming a small bump means no problem
- Stopping your medication because you’re scared of bleeding
- Not telling the ER team you’re on blood thinners
- Ignoring dizziness or nausea because "it’s just a headache"
One of the biggest errors is assuming the Canadian CT Head Rule applies to you. That rule was made for healthy people with minor head injuries. It’s not meant for anyone on anticoagulants. Using it could miss up to 15% of serious bleeds.
What to Expect at the Emergency Room
When you arrive, they’ll check your vital signs and ask about your medication. They’ll want to know:
- What blood thinner you take (name and dose)
- When you last took it
- If you’ve had any recent falls or injuries
- Any history of brain bleeds or strokes
You’ll likely get a blood test-PT, INR, and type and screen-to check how well your blood clots. If your INR is too high (over 3.5 on warfarin), they may give you vitamin K or a clotting agent like PCC. If you’re on a DOAC like apixaban, they might use Idarucizumab (Praxbind) to reverse it quickly.
Then comes the CT scan. It’s fast-usually under 10 minutes. No needles, no pain. Just lie still while the machine takes pictures.
When to Go Back to the ER
If you’re sent home after a normal scan, you still need to watch for warning signs. Call 000 or go back to the ER immediately if you develop:
- A headache that gets worse instead of better
- Confusion, trouble recognizing people, or memory loss
- Weakness or numbness in your arm, leg, or face
- Slurred speech or trouble understanding others
- Seizures
- Vomiting more than twice
- Drowsiness or difficulty waking up
These aren’t "maybe" signs. They’re red flags. Even if it’s 2 a.m. or you think you’re overreacting-go. Delayed bleeds don’t wait for business hours.
What’s Changing in 2025
Doctors are starting to look beyond CT scans. Blood tests that detect brain proteins like UCH-L1 and GFAP (the Banyan Brain Trauma Indicator) are being studied to help decide who really needs a scan. Early results show promise, especially for older adults with mild symptoms.
Also, researchers are working on a modified version of the Canadian CT Head Rule specifically for people on DOACs. It’s expected to be ready in 2025. Until then, the safest rule is simple: if you’re on blood thinners and you hit your head, get scanned.
And if you’re over 65, living alone, or have a history of falls, talk to your doctor about fall prevention. The CDC’s STEADI program offers tools to reduce fall risk-like checking your vision, removing rugs, and reviewing medications that make you dizzy. Preventing the fall is just as important as treating the injury.
Frequently Asked Questions
Do I need a CT scan if I didn’t lose consciousness after hitting my head?
Yes. Losing consciousness is just one of many warning signs. Many people on blood thinners develop brain bleeds without ever passing out. If you had a direct blow to the head, fell from a height, are over 65, or have any confusion or vomiting, you need a CT scan-even if you feel fine.
Can I wait a few hours to see if I feel worse?
No. Delaying imaging increases the risk of complications. Bleeds can grow silently. By the time you feel worse, the damage may be irreversible. Emergency departments prioritize anticoagulated patients for immediate CT scans because time saves lives.
Should I stop taking my blood thinner after a head injury?
Never stop your blood thinner without medical advice. Stopping can cause a stroke or clot. If you have a bleed, doctors will decide whether to reverse the anticoagulant using specific medications like PCC or Idarucizumab. This decision requires expert input-don’t make it yourself.
Is an MRI better than a CT scan for detecting brain bleeds?
CT is the first-line test because it’s fast, widely available, and excellent at spotting fresh blood. MRI is more sensitive for small or old bleeds but takes longer and isn’t always available in emergencies. It may be used later for follow-up in stable patients, but never as the first step.
What if I’m on aspirin instead of a stronger blood thinner?
Aspirin is still an antiplatelet drug and increases bleeding risk-even if less than warfarin or DOACs. Guidelines treat aspirin users the same as other anticoagulated patients when it comes to head injury. If you’re on daily aspirin and hit your head, get scanned.
How long should I be monitored after a normal CT scan?
Most hospitals recommend at least 6 hours of observation. Some, especially for older adults or those with other health issues, keep patients for 24 hours. Even if you’re discharged, you must watch for symptoms for the next 72 hours. Delayed bleeds can happen up to three days after injury.
What to Do Next
If you’re on blood thinners, keep a card or note in your wallet that lists your medication, dose, and doctor’s contact info. Wear a medical alert bracelet if you can. Talk to your doctor about fall prevention-especially if you’re older or have balance issues.
If you’ve recently had a head injury and haven’t been scanned yet, go to the ER now. Don’t wait. Don’t call your GP first. Go straight to the nearest emergency department. Tell them you’re on blood thinners. That one phrase changes everything.
Head injuries on blood thinners aren’t about being overly cautious. They’re about survival. The scan takes minutes. The risk of waiting? It’s not worth it.


Shawna B
December 3, 2025 AT 23:18Just got bumped on the head yesterday and didn’t think twice. Now I’m sweating bullets reading this. Go get scanned. No excuses.
vanessa parapar
December 4, 2025 AT 13:08Oh honey, I’ve been telling people this for years. You think a little bump’s nothing? Sweetie, I’ve seen three people in my circle go from ‘I’m fine’ to ‘Why is my vision blurry?’ in six hours. CT scan isn’t optional-it’s your lifeline. And if you’re on aspirin? Same rules. Don’t be that person who waits and then blames the ER for not saving you. You knew better.
Jerry Ray
December 6, 2025 AT 04:38Actually, the data’s way overstated. I’ve seen way too many CTs done on people who were perfectly fine. The real problem is overtesting leading to unnecessary radiation and costs. Not everyone needs a scan. Some of us have been on blood thinners for a decade and never had an issue. Maybe we should stop treating every bump like a nuclear event.
David Ross
December 7, 2025 AT 05:29And yet, here we are-another liberal, fear-mongering, overcautious medical guideline that treats adults like children. In my day, you got up after a fall, wiped the blood off, and kept going. Now? You need a scan because you stubbed your toe on the coffee table? This is why America’s healthcare is broke. You’re not a fragile porcelain doll. Stop coddling yourselves.
Abhi Yadav
December 7, 2025 AT 20:46Life is a river... and blood thinners? They just make the current stronger. But the mind... the mind is the true vessel. When you hit your head, you don't just risk bleeding-you risk the echo of your soul hitting the walls of your skull. 🌊🧠 Maybe the scan is not for the brain... but for the heart that fears it's already too late.
Krys Freeman
December 9, 2025 AT 15:02Another waste of taxpayer money. If you're dumb enough to fall and are on blood thinners, you shouldn't be driving, let alone living alone. Let the insurance company pay for your stupidity.
AARON HERNANDEZ ZAVALA
December 9, 2025 AT 15:15I get why this feels scary. I had a fall last year and panicked for weeks. But reading this made me realize-this isn’t about fear. It’s about being smart. I didn’t get scanned right away either. I wish I had. I’m so glad someone laid this out so clearly. Thank you. I’ll keep the med card in my wallet now. And I’m talking to my doctor about fall risks. No more rugs.
Lyn James
December 10, 2025 AT 14:27Let me just say this-this entire post is a masterpiece of responsible medical communication. I’ve been a nurse for 27 years, and I’ve seen too many people die because they thought ‘it was just a bump.’ I’ve held the hands of families who begged for one more hour, one more chance. And you know what? The ones who waited? They never got it. The ones who went straight to the ER? They lived. This isn’t fearmongering. This is compassion wrapped in science. And if you’re the kind of person who reads this and says ‘I’ll wait,’ you’re not just risking your life-you’re risking the peace of mind of everyone who loves you. I’ve watched mothers cry because their 70-year-old dad didn’t get a scan. Don’t be that person. Don’t be the reason someone’s last memory of you is a hospital room with no answers. Get scanned. No debate. No ‘maybe.’ Just go. Now. Before it’s too late.