How Generic Medications Save Trillions in Healthcare Costs
 Jan, 1 2026
Jan, 1 2026
Every year, Americans fill over 3.9 billion prescriptions for generic medications. That’s nine out of every ten prescriptions written. And yet, these generics make up just 12% of total drug spending. The rest-$700 billion in 2024 alone-went to brand-name drugs, even though they’re prescribed far less often. This isn’t a glitch. It’s the system working exactly as designed. And it’s saving the U.S. healthcare system over $467 billion a year.
How Generics Cut Costs So Dramatically
Generic drugs aren’t cheaper because they’re low quality. They’re cheaper because they don’t need to repeat the billion-dollar clinical trials that brand-name drugs do. Once a patent expires, other manufacturers can copy the active ingredient, prove it works the same way, and sell it for a fraction of the price. The FDA requires generics to have the same strength, dosage, safety, and effectiveness as the brand. No exceptions. Take lisinopril, a blood pressure pill. The brand version, Zestril, used to cost over $100 a month. Today, the generic version? Around $4. Same active ingredient. Same side effects. Same results. That’s a 96% drop in price. Multiply that across hundreds of common drugs-metformin for diabetes, atorvastatin for cholesterol, levothyroxine for thyroid-and you start to see why the savings add up so fast. In 2024, the top 10 most prescribed generic drugs saved patients and insurers $89.5 billion. The top 10 with the highest total savings? They saved $127 billion. That’s not a typo. Just ten medications accounted for nearly a third of all generic savings that year.Biosimilars: The Next Wave of Savings
Biosimilars are the next frontier. These aren’t exact copies like traditional generics-they’re highly similar versions of complex biologic drugs made from living cells. Think drugs like Humira, Enbrel, or insulin analogs. These used to cost $5,000 to $10,000 a year per patient. Now, biosimilars are entering the market and cutting those prices by 30-50%. Since the first biosimilar hit the U.S. market in 2015, they’ve saved $56.2 billion. In 2024 alone, they saved $20.2 billion. That’s not just a win for patients-it’s a lifeline for Medicare and Medicaid. Without biosimilars, the cost of treating autoimmune diseases, cancer, and diabetes would be skyrocketing even faster than it already is.Why the U.S. Saves More Than Other Countries
The U.S. fills 90% of prescriptions with generics. Most European countries hover around 60-80%. So why do Americans still pay more for drugs overall? It’s not because generics are expensive here. It’s because brand-name drugs are wildly overpriced. In Canada, Germany, or Australia, the same brand-name drug might cost half as much. But in the U.S., brand manufacturers use legal loopholes to delay competition. They file dozens of patents on minor changes-like a new pill shape or a slightly different coating-to extend their monopoly. This is called “patent thickets.” A 2024 study found that just four brand-name drugs, protected by these tactics, cost the system over $3.5 billion in lost savings over two years. Another tactic, called “product hopping,” involves switching patients from an older drug to a new version right before the patent expires-so generics can’t enter until the new patent runs out. These aren’t theoretical problems. They’re real, documented strategies that keep prices high. The Congressional Budget Office estimates that stopping these practices could save $1.8 billion over ten years. That’s money that could go to more patients, not corporate profits.
Who’s Really Saving Money?
The biggest winners? Patients on Medicare and Medicaid. In 2024, generics saved Medicare $142 billion and Medicaid $62.1 billion. That’s not just a number-it’s thousands of seniors who didn’t have to choose between their medication and their groceries. It’s children with asthma who got their inhalers instead of going without. Private insurers saved too. Express Scripts, one of the largest pharmacy benefit managers, reported $18.3 billion in savings from generic substitution in 2023 alone. That’s money that flows back into lower premiums, better coverage, or more services. But here’s the catch: not everyone benefits equally. Some patients still pay high out-of-pocket costs for generics because of how insurance plans are structured. A 2023 survey found that 42% of patients abandoned prescriptions due to cost-even when generics were available. Why? Because some plans still push higher-cost brand drugs through formularies, or require prior authorization just to fill a generic.Barriers to Full Savings
The system is broken in places, even when the solution is clear. Pharmacy Benefit Managers (PBMs) are supposed to negotiate lower prices. But sometimes they get paid more to promote brand-name drugs over generics. That’s called a “rebate trap.” It’s legal, but it undermines savings. Then there’s administrative red tape. Prior authorization requirements for generics jumped 47% between 2019 and 2023. That means doctors spend more time filling out forms, and patients wait longer to get their meds-even when a generic is available and cheaper. Some states are fighting back. California’s Generic Drug Discount Program mandates pharmacists to substitute generics unless the doctor says no. Result? 98% generic utilization. Texas, with a more relaxed policy, sits at 87%. The difference? Billions in savings.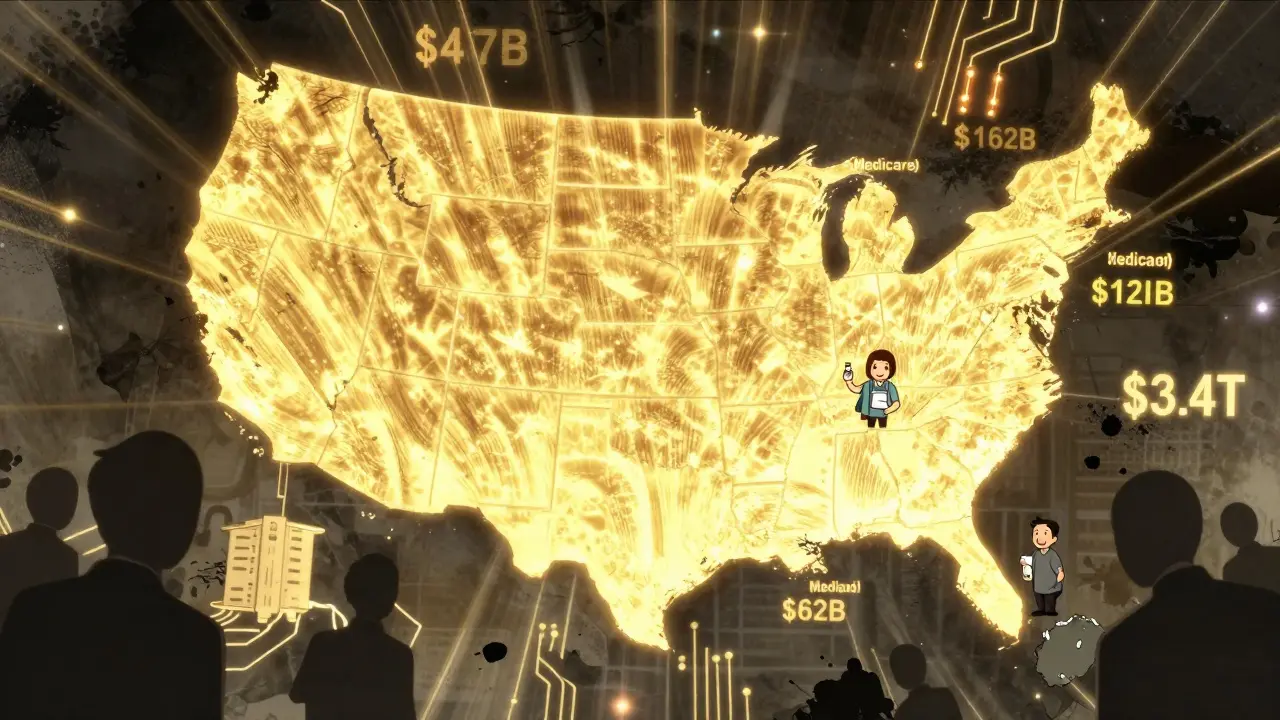
What’s Next?
The FDA approved 1,145 new generic drugs in 2024-up 7.3% from the year before. Another $24 billion in drug spending is expected to open up to generics by 2025. That includes complex injectables, inhalers, and other high-cost treatments. Legislation like S.1041, the Affordable Prescriptions for Patients Act, passed the Senate HELP Committee in 2024 with bipartisan support. If enacted, it would crack down on patent abuse and could save $7.2 billion annually. But challenges remain. Drug shortages hit 287 generic medications in December 2024-many due to manufacturing issues overseas. And the market is consolidating: the top 10 generic manufacturers now control 63% of the market, up from 51% in 2015. Less competition means less downward pressure on prices.What Patients Can Do
You don’t need to wait for Congress to act. Here’s what you can do right now:- Ask your doctor: “Is there a generic version?” Always. Even if you’ve been on a brand drug for years, a generic may now be available.
- Check your insurance formulary. If your plan prefers a brand over a cheaper generic, ask for a prior authorization exception.
- Use mail-order pharmacies or discount programs like GoodRx. Even if your insurance doesn’t cover a generic fully, you can often pay less out-of-pocket through these services.
- Speak up. If your pharmacy won’t substitute a generic without your permission, ask why. In most states, pharmacists are required to substitute unless the prescriber says no.
The Bigger Picture
The U.S. spends $4.9 trillion on healthcare each year. Prescription drugs make up about 10% of that-$490 billion. Generics and biosimilars saved $467 billion in 2024. That’s nearly the entire drug budget covered by savings from cheaper alternatives. Think about that. We’re not talking about small savings. We’re talking about a system where the cheapest, safest, most effective option is also the most underused because of corporate incentives and bureaucratic barriers. The data doesn’t lie. Generics work. They save lives. They save money. And they’ve already saved $3.4 trillion over the last decade. The question isn’t whether we can afford generics. It’s whether we can afford not to use them.Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for purity, stability, and bioavailability. In clinical terms, they are considered therapeutically equivalent. While some patients report minor differences in side effects or how they feel-often due to inactive ingredients like fillers or dyes-these are rare and not due to the medication’s effectiveness. Over 87% of patients who use generics rate cost as excellent or good, and most report no difference in how well the drug works.
Why do some pharmacies refuse to substitute generics?
In most states, pharmacists are legally allowed-and often required-to substitute a generic unless the doctor writes “dispense as written” or “no substitution.” If a pharmacy refuses, it’s often because of how their contract with the pharmacy benefit manager (PBM) is structured. Some PBMs incentivize pharmacies to push brand-name drugs through rebates. Patients can ask the pharmacist to check if substitution is allowed under state law, or ask their doctor to clarify the prescription. If you’re being denied a generic without a clear reason, you have the right to ask why.
Do biosimilars save as much as traditional generics?
Not yet-but they’re catching up fast. Traditional generics can be 80-95% cheaper than brand drugs because they’re chemically identical and easier to produce. Biosimilars are more complex and costlier to develop, so they typically save 15-35% compared to the original biologic. But since biologics cost $5,000-$10,000 a year, even a 30% savings means thousands of dollars per patient. Since 2015, biosimilars have already saved $56.2 billion in the U.S., and that number is growing rapidly. Experts predict they’ll save over $100 billion in the next decade as more enter the market.
Why are generic drugs still expensive for some people?
Even though generics are cheap to make, their price at the pharmacy isn’t always low. That’s because of how insurance and pharmacy benefit managers (PBMs) set prices. Some plans have high copays for generics, especially if they’re not on the preferred list. Others require prior authorization, which delays access. In 2023, nearly half of patients who couldn’t afford their meds switched to generics-and 89% of them reported satisfaction with both cost and effectiveness. But if your plan doesn’t cover a generic well, you can often pay less using discount programs like GoodRx, SingleCare, or RxSaver, which can drop the price to $5 or less for common medications.
What’s the biggest threat to future generic savings?
The biggest threats are patent abuse and manufacturing consolidation. Brand-name companies are filing more patents on minor changes to delay generic entry. At the same time, the generic market is shrinking: the top 10 manufacturers now control 63% of the market, up from 51% in 2015. Fewer competitors mean less pressure to lower prices. Drug shortages are also a growing concern-with 287 generic medications in short supply as of late 2024-often due to production issues overseas. Without policy changes to curb anti-competitive behavior and support domestic manufacturing, the pace of savings could slow.

