Hyponatremia from SSRIs: How Low Sodium and Confusion Risk Affect Antidepressant Use
 Nov, 25 2025
Nov, 25 2025
When you start an SSRI for depression, you expect better mood, more energy, maybe better sleep. You don’t expect to become confused, nauseous, or stumble like you’re drunk. Yet for some people-especially older adults-this is exactly what happens. It’s not dementia. It’s not aging. It’s hyponatremia-a dangerous drop in blood sodium caused by the very medication meant to help.
What Is Hyponatremia, Really?
Hyponatremia means your blood sodium level has fallen below 135 mmol/L. Sodium isn’t just table salt. It’s a key electrolyte that keeps your nerves, muscles, and brain working right. When sodium drops too low, water floods into your cells-including brain cells. That’s when confusion, dizziness, headaches, and seizures start. In severe cases, sodium can plunge to 118 mmol/L or lower, leading to coma or death.This isn’t rare. A 2024 meta-analysis in European Psychiatry found that 1.9% to 4.4% of people taking SSRIs develop hyponatremia. But for those over 65? The risk jumps to nearly 1 in 6. That’s not a small side effect. It’s a major clinical hazard.
Why Do SSRIs Cause Low Sodium?
SSRIs boost serotonin in your brain to fight depression. But serotonin doesn’t just stay in the brain. It also triggers the release of antidiuretic hormone (ADH), which tells your kidneys to hold onto water. Normally, your body balances water and sodium. But too much ADH? Your kidneys keep water, dilute your blood, and sodium levels crash.This is called SIADH-Syndrome of Inappropriate Antidiuretic Hormone Secretion. It’s not a mistake. It’s a direct pharmacological effect. The stronger the SSRI binds to the serotonin transporter (SERT), the higher the risk. That’s why citalopram and sertraline carry the highest risk, followed by fluoxetine and paroxetine.
It’s not just the drug. It’s who’s taking it. Women, people under 60 kg, those with kidney issues (eGFR below 60), and anyone on diuretics-especially thiazides-are at much higher risk. Combine SSRI with a water pill? Your hyponatremia risk shoots up 4.2 times.
When Does It Happen?
Most cases show up within two to four weeks of starting the SSRI-or after a dose increase. That’s why many doctors miss it. They assume confusion in an elderly patient is just dementia. Or they think nausea is just stomach flu. The symptoms are subtle at first: fatigue, headache, feeling off. Then it escalates: disorientation, falls, seizures.A 78-year-old woman in a 2022 case report started sertraline at 50 mg daily. Ten days later, her sodium dropped to 118 mmol/L. She ended up in the ICU. Another case from Reddit: an 82-year-old woman on citalopram became so confused her family thought she had a stroke. Her sodium? 122 mmol/L. She needed hospitalization. Both cases were misdiagnosed for days.
On average, it takes 7.2 days from symptom onset to the correct diagnosis. That’s a lot of time for brain swelling to happen.
Who’s at Highest Risk?
It’s not random. Certain people are far more vulnerable:- Age 65+: Risk is 3.7 times higher than younger adults
- Women: 65% of reported cases are female
- Low body weight: Under 60 kg increases susceptibility
- Chronic kidney disease: eGFR below 60 means less ability to excrete excess water
- On diuretics: Especially hydrochlorothiazide
- Multiple medications: Polypharmacy increases interaction risk
And here’s the kicker: only 28.7% of patients report being told about this risk before starting SSRIs. That’s not informed consent. That’s negligence.
How Do Doctors Miss It?
A 2023 survey in The Carlat Report found that 63.4% of primary care doctors didn’t know hyponatremia typically develops 2-4 weeks after starting an SSRI. Many assume symptoms are behavioral or neurological decline. In nursing homes, hyponatremia is often chalked up to “getting older.”But the signs are there. If an elderly patient suddenly becomes confused, falls more often, or loses appetite, check their sodium. It’s a simple blood test. Yet, in 37.8% of mild cases, it goes undetected in primary care. That’s why so many end up in the ER-or worse.
What About Other Antidepressants?
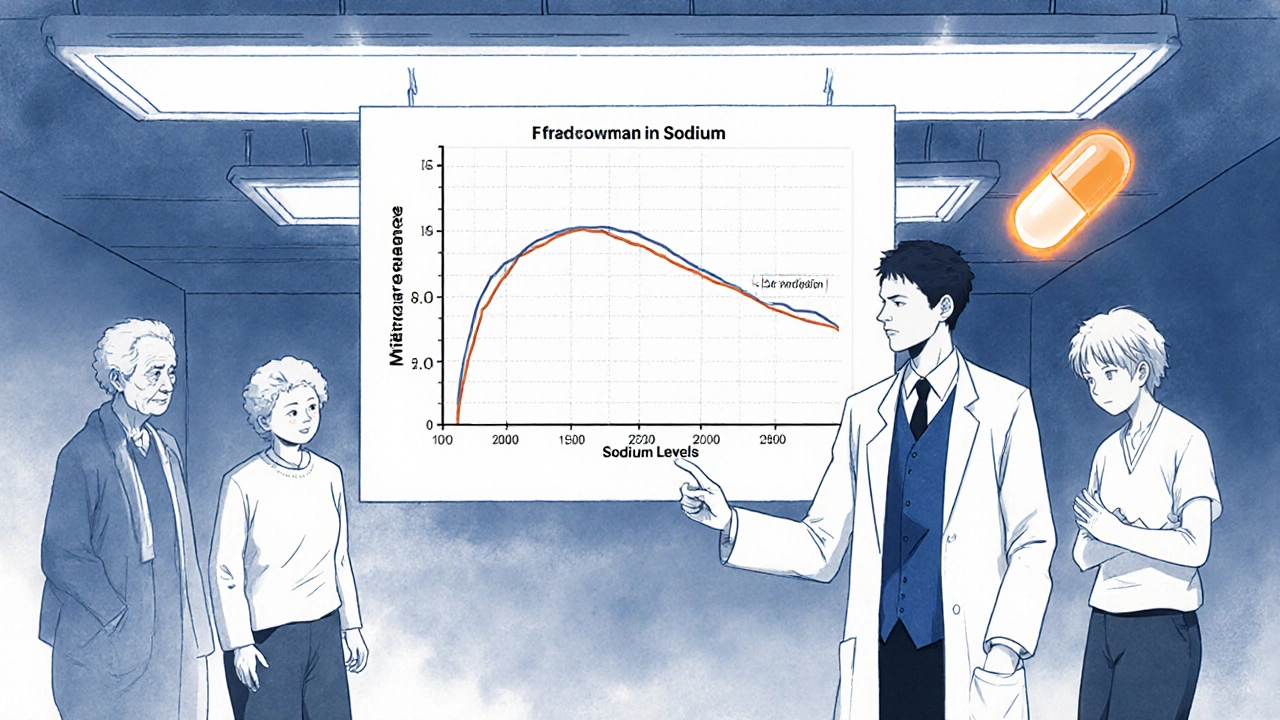
Not all antidepressants are equal when it comes to sodium risk.SSRIs as a class have 2.86 times higher risk than non-SSRIs. But some alternatives are much safer:
| Medication | Risk Relative to SSRIs | Notes |
|---|---|---|
| Citalopram | 2.37x | Highest risk SSRI |
| Sertraline | 2.15x | Commonly prescribed, high risk |
| Fluoxetine | 1.98x | Long half-life, risk lingers |
| Paroxetine | 1.82x | Also anticholinergic, adds confusion risk |
| Venlafaxine (SNRI) | 1.72x | Moderate risk |
| Amitriptyline (TCA) | 1.94x | Higher risk than nortriptyline |
| Bupropion | 0.85x | Lower risk, no serotonin effect |
| Mirtazapine | 0.47x | Lowest risk-recommended for elderly |
For older adults, mirtazapine is now the preferred first-line option. It doesn’t affect serotonin the same way. No SIADH. No water retention. No sodium crash. Studies show that for every 1,000 elderly patients switched from SSRIs to mirtazapine, you prevent 12 cases of hyponatremia. That’s not just safer-it’s life-saving.
What Should You Do?
If you or a loved one is on an SSRI, especially if over 65, here’s what you need to do:- Ask for a baseline sodium test before starting the medication.
- Get it repeated at 2 weeks after starting or increasing the dose.
- Watch for early signs: Headache, nausea, fatigue, mild confusion.
- Don’t assume it’s aging. Confusion in the elderly is not normal.
- Ask about alternatives. Is mirtazapine or bupropion an option?
- Report any changes to your doctor immediately-even if they seem minor.
The American Psychiatric Association and American Geriatrics Society now recommend sodium testing before and within two weeks of starting antidepressants in older adults. This isn’t optional. It’s standard care.
What Happens If It’s Diagnosed?
If sodium is below 135 mmol/L and symptoms are present:- Mild (125-134 mmol/L): Stop the SSRI. Restrict fluids to 800-1,000 mL per day. Sodium usually normalizes in 3-4 days.
- Severe (<125 mmol/L): Hospitalization. IV hypertonic saline (3%) at controlled rates. Too fast? You risk osmotic demyelination-a permanent brain injury.
Recovery takes time. Even after sodium normalizes, brain fog and balance issues can linger for weeks. That’s why prevention matters more than treatment.
The Bigger Picture
SSRIs are still the most prescribed antidepressants in the U.S.-over 214 million prescriptions in 2023. But prescribing patterns are shifting. Between 2018 and 2023, SSRI use in patients over 65 dropped by 22.3%. Meanwhile, mirtazapine prescriptions for seniors rose by 34.7%.The cost? $1.27 billion annually in the U.S. for hospitalizations and ER visits tied to SSRI-induced hyponatremia. That’s not just a medical issue. It’s a financial and human crisis.
The FDA now requires SSRI labels to include hyponatremia warnings. The European Medicines Agency is reviewing safety data. And by 2027, mirtazapine is projected to be the top antidepressant for patients over 65.
Final Thought
Antidepressants save lives. But they can also harm-especially when we ignore the science. Hyponatremia isn’t a rare side effect. It’s a predictable, preventable danger. For younger adults with no other health issues, the benefits often outweigh the risks. But for older adults? The math changes.There’s no reason to risk confusion, falls, or brain damage when safer alternatives exist. Ask the questions. Demand the test. Push for the right medication. Your brain-and your life-deserve nothing less.
Can SSRIs cause confusion in elderly patients?
Yes. SSRIs can cause confusion in elderly patients due to hyponatremia-a drop in blood sodium levels caused by excessive water retention. This typically happens within 2-4 weeks of starting the medication. Symptoms like disorientation, dizziness, and memory problems are often mistaken for dementia or aging, but they’re medical emergencies that require immediate sodium testing.
Which SSRIs have the highest risk of causing low sodium?
Citalopram carries the highest risk, followed by sertraline, fluoxetine, and paroxetine. These SSRIs have strong binding affinity to the serotonin transporter, which triggers excessive antidiuretic hormone release, leading to water retention and diluted sodium levels. Citalopram’s risk is 2.37 times higher than non-SSRI antidepressants.
Is mirtazapine safer than SSRIs for older adults?
Yes. Mirtazapine has the lowest risk of hyponatremia among antidepressants-just 47% of the risk seen with SSRIs. It doesn’t stimulate antidiuretic hormone like SSRIs do. Major guidelines, including the American Geriatrics Society Beers Criteria, now recommend mirtazapine as a first-line alternative for elderly patients needing antidepressant therapy.
Should I get my sodium checked before starting an SSRI?
If you’re over 65, have kidney issues, take diuretics, or are underweight, yes. The American Psychiatric Association recommends baseline sodium testing before starting any SSRI in high-risk patients, followed by a repeat test at 2 weeks. This simple step can prevent hospitalization and brain injury.
How long does it take for sodium levels to return to normal after stopping an SSRI?
In mild cases, sodium levels typically normalize within 72 to 96 hours after stopping the SSRI and restricting fluids. In severe cases requiring hospitalization, correction takes longer and must be done slowly to avoid permanent brain damage. Full neurological recovery can take days to weeks, even after sodium is normal.
Can hyponatremia from SSRIs be fatal?
Yes. When serum sodium falls below 125 mmol/L, it can lead to seizures, coma, respiratory arrest, and death. Severe cases require emergency treatment with hypertonic saline. The risk is highest in elderly patients, especially those on multiple medications or with pre-existing kidney disease.


Brittany Medley
November 25, 2025 AT 19:05Just had my 79-year-old mom on sertraline for 3 weeks - started stumbling, forgetting names, nausea. We thought it was early dementia. Blood test showed sodium at 121. Stopped the med, fluids restricted, she’s back to normal in 5 days. Why isn’t this standard protocol? Doctors act like it’s a surprise every time.
Asia Roveda
November 26, 2025 AT 12:36Of course SSRIs cause hyponatremia - big pharma doesn’t care if old people turn into walking zombies as long as they keep buying pills. They market these like candy. No one tells you the real risks because the lawsuits are buried under NDAs. This isn’t medicine, it’s corporate murder with a prescription pad.
Micaela Yarman
November 27, 2025 AT 01:40It is deeply concerning that the medical community continues to under-recognize this potentially fatal adverse effect. The data presented here is unequivocal, and the failure to implement mandatory sodium monitoring in elderly patients constitutes a systemic breach of the duty of care. This must be addressed through policy reform, not merely anecdotal awareness.
mohit passi
November 28, 2025 AT 11:18Deborah Williams
November 28, 2025 AT 19:27Wow. So the same doctors who tell us to "just take the pill" and "don’t worry about side effects" are the ones who then shrug when Grandma starts hallucinating? Let me guess - they blame it on "old age" again. Classic. I bet they also think depression is just being sad and you should "snap out of it."
Kaushik Das
November 30, 2025 AT 17:39Man, I never knew SSRIs could do this. I thought they were just mood boosters. But this? This is straight-up brain flooding. I’m switching my pops from sertraline to mirtazapine next week - no way I’m risking him turning into a confused mess. Also, that table? Chef’s kiss. Saved it. Will share with my nurse aunt.
Cynthia Springer
December 2, 2025 AT 01:26Is this only a problem with SSRIs? What about SNRIs like venlafaxine? I’m on that one and I’ve had weird headaches since starting. Could it be this? I’m 68, female, 58kg, and on hydrochlorothiazide… I’m starting to panic.
Ali Miller
December 2, 2025 AT 20:49THIS IS WHY AMERICA IS FALLING APART. Our elderly are being drugged into oblivion by overworked doctors who don’t even check basic labs. They’re too busy chasing productivity quotas to care if you live or die. This isn’t health care - it’s a profit-driven assembly line. And you? You’re just a number on a spreadsheet.
JAY OKE
December 4, 2025 AT 11:00My grandma was on citalopram for 2 months. One day she just stopped eating, started mumbling, couldn’t walk straight. We took her to the ER and they found her sodium at 119. They said "this happens sometimes." Like it’s normal? I’m done trusting doctors to just wing it.
Stephen Adeyanju
December 5, 2025 AT 20:04Why are they even prescribing these to old people in the first place? They don’t need antidepressants they need to be left alone and given more soup and hugs
james thomas
December 5, 2025 AT 22:29Big Pharma knows this. They’ve known since the 90s. They buried the studies. They lobbied against warnings. They even got the FDA to delay labeling changes. This isn’t an accident. It’s a calculated risk. Elderly people die quietly. No one complains. No lawsuits. Just another statistic.
Rachel Whip
December 7, 2025 AT 13:00Thank you for sharing this. I’m a geriatric nurse and I see this every month. We test sodium routinely now - after your post, we made it protocol. If you’re on an SSRI and over 65, we test at baseline, week 2, and week 4. It’s not optional. It’s basic. And if sodium drops? We switch immediately. No waiting. No "wait and see." Lives saved.
Ezequiel adrian
December 9, 2025 AT 01:52Bro I’m from Nigeria and we don’t even have basic labs in most clinics. Imagine this happening here. No tests. No follow-up. Just pills. People die. No one knows why. This needs to be shouted from rooftops - especially in developing countries.
Joe bailey
December 9, 2025 AT 11:22Just had my dad switch from sertraline to mirtazapine last month. He went from "I don’t know who I am anymore" to "I think I’ll have pancakes tomorrow." I’m so grateful. Please, if you’re on an SSRI and over 60 - ask for sodium. It’s a 5-minute test. Could save your life.