Language Barriers and Medication Safety: How to Get Help
 Feb, 3 2026
Feb, 3 2026
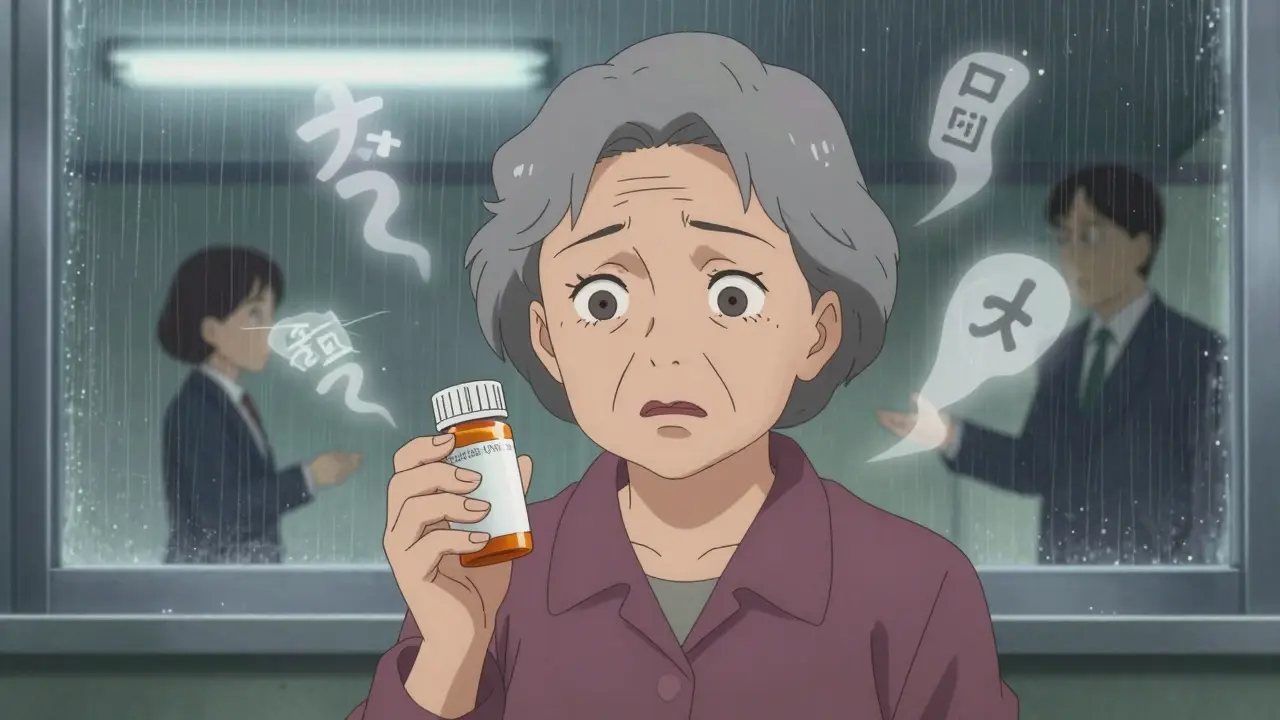
When Your Medication Instructions Don’t Make Sense
You’ve been given a new prescription. The pharmacist hands you a bottle with tiny print. You nod along, pretending you understand the instructions. But you don’t. The words on the label mean nothing. You’re not sure if you’re supposed to take it before food or after. Is it once a day or three times? What does dropperful even mean? This isn’t just confusing-it’s dangerous. For millions of people with limited English proficiency, this is everyday reality. And the consequences? Hospital visits, overdoses, missed doses, and even death.
Studies show that patients who can’t communicate clearly with their healthcare providers are twice as likely to have a medication error. Children in LEP (Limited English Proficiency) families face a 17.7% risk of adverse drug events-nearly double the rate of English-speaking families. These aren’t rare cases. They’re systemic failures.
Why Language Barriers Are Deadly
It’s not just about not understanding the word tablet or daily. It’s about missing critical details. A Spanish-speaking parent might hear every 6 hours but the label says every 8 hours. A Vietnamese patient might be told to take a pill with water, but the pharmacist meant with food-and the drug causes stomach bleeding on an empty stomach. These aren’t misunderstandings. They’re preventable medical errors.
One Reddit user shared how their mother was given insulin instructions through Google Translate. The app misread 10 units as 1 unit. The result? A trip to the ER. Another case from a Milwaukee pharmacy found that half of the pharmacies there never printed prescription labels in Spanish-even though 60% of their patients spoke Spanish. That’s not an accident. It’s negligence.
And it’s not just pharmacies. Hospitals, clinics, and even telehealth platforms are failing. A 2023 University of Michigan study found that 29% of hospitals don’t offer any online language services-even though more care is moving digital. If you can’t access your prescription instructions in your language, you’re being left behind.
What Actually Works: Professional Interpreters
Using family members, friends, or Google Translate isn’t just risky-it’s reckless. A 2022 NCBI study found that up to 25% of interpretations done by untrained people contain serious medical errors. A child translating for their parent might not know what anticoagulant means. A neighbor might say take two when the doctor said take one every 12 hours.
Professional medical interpreters-whether in person, over the phone, or via video-cut medication errors by up to 50%. They’re trained in medical terminology. They know how to convey dosage instructions accurately. They don’t guess. They don’t simplify. They translate precisely.
One hospital in Pennsylvania saw a 40% drop in medication errors within a year after hiring professional interpreters for every LEP patient visit. That’s not luck. That’s policy working. And it’s not expensive. Phone interpretation services cost as little as $3.50 per minute. Video interpretation runs $4-$6 per minute. For a 15-minute consultation? That’s less than the cost of a coffee.

What Hospitals and Pharmacies Should Be Doing
By law, any healthcare provider receiving federal funds-like Medicare or Medicaid-must provide language assistance. That’s not optional. It’s Title VI of the Civil Rights Act. Yet, a 2023 report found that 68% of hospitals still can’t identify LEP patients before they arrive. That’s like handing out a life jacket after someone’s already in the water.
Here’s what works:
- Ask everyone at intake-not just those who “look” like they might need help. Use a simple question: “What language do you speak at home?” Put it on every form, every kiosk, every website.
- Use certified interpreters for every clinical interaction, especially when discussing medications. No exceptions.
- Translate high-risk instructions-insulin, blood thinners, seizure meds-into the top 5-10 languages spoken in your area. Don’t wait for someone to ask.
- Use the teach-back method. After explaining, ask the patient: “Can you show me how you’ll take this pill?” If they can’t, you haven’t communicated yet.
- Offer directly observed dosing for complex meds. Have a nurse watch the patient take the first dose. It takes 5 minutes. It prevents a lifetime of regret.
Some pharmacies now print bilingual labels. Some EHR systems automatically flag language preferences. Epic and Cerner, the two biggest health software companies, rolled out updated language modules in 2024. But adoption is slow. Only 31% of pharmacies in the Bronx can print Spanish labels. That’s not progress. That’s failure.
What You Can Do Right Now
If you or someone you care for has limited English proficiency, here’s how to protect yourself:
- Ask for an interpreter-even if no one offers. Say: “I need a professional interpreter to understand my medicine.” You have a legal right to one.
- Don’t rely on family for complex meds. Even if they’re fluent, they’re not trained. A child shouldn’t be translating insulin doses.
- Take your pill bottle to the pharmacy and ask them to explain it out loud in your language. If they can’t, ask for a supervisor.
- Use the teach-back method yourself. After the pharmacist explains, say: “So, I take this one pill every morning with breakfast, right?” If they nod, you’re good. If they hesitate, ask again.
- Know your rights. If you’re denied an interpreter, file a complaint with the Office for Civil Rights. Penalties for noncompliance can reach $100,000 per violation.
There are apps now that translate medication labels in real time-like MedSavvy and HealthLingo. But don’t trust them alone. Use them as a backup, not a replacement for human interpretation.
Why This Isn’t Just About Language
This is about dignity. About safety. About equity.
Dr. Urmimala Sarkar, who led the 2022 study on pediatric medication errors, said it plainly: “From an equity standpoint, these disparities are not acceptable.” We wouldn’t let someone with a visual impairment read a tiny label without a magnifier. Why are we letting someone with a language barrier take a pill without a translator?
Language isn’t just words. It’s trust. It’s control. It’s life.
When you can’t understand your medicine, you’re not just confused-you’re vulnerable. And that vulnerability is exploited by a system that assumes everyone speaks the same language. It’s time to fix that.
What’s Changing-and What’s Next
The good news? Things are moving. In 2023, Medicare started reimbursing for telehealth interpretation. In 2024, the FDA plans to release new rules requiring multilingual labeling on high-risk medications. The NIH is funding AI tools that can translate dosage instructions with medical accuracy-not just word-for-word, but meaning-for-meaning.
But change won’t happen unless people demand it. The market for healthcare language services is growing fast-projected to hit $2 billion by 2028. That means companies are investing. That means hospitals can afford to act. But only if they’re held accountable.
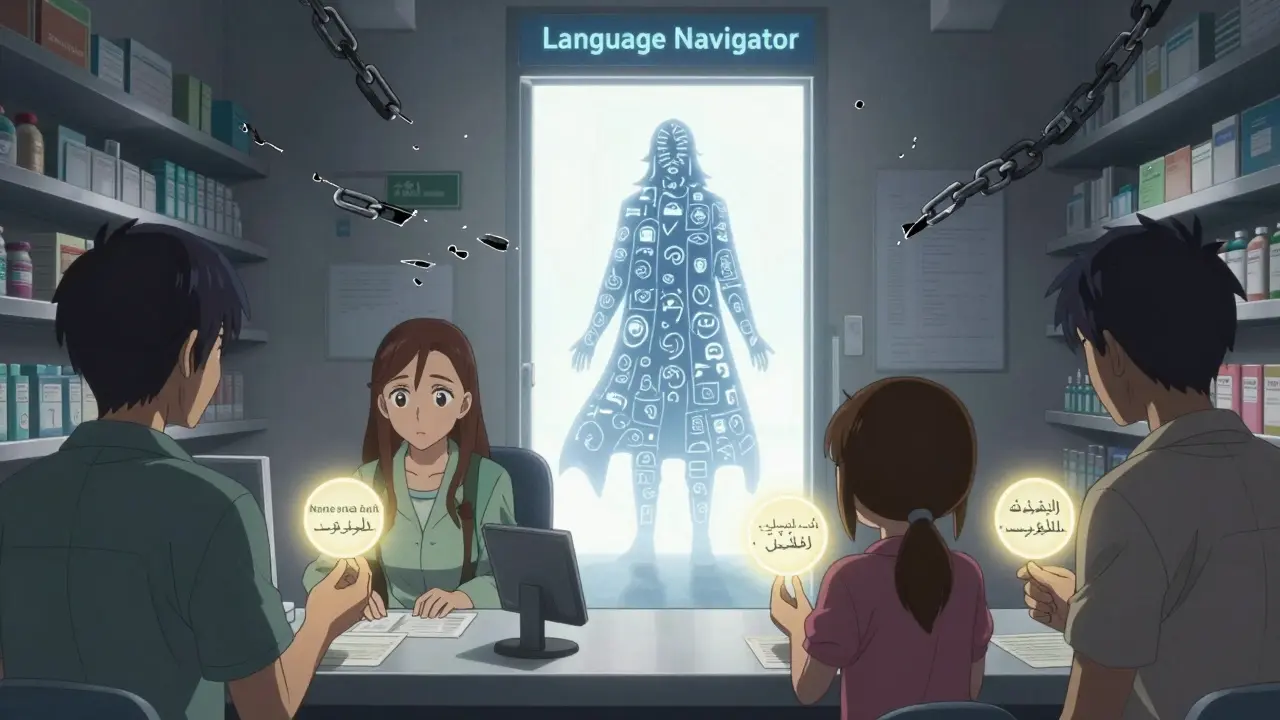
Community health centers are starting interpreter training programs. Hospitals are hiring bilingual pharmacists. Some clinics now have “language navigators”-staff whose only job is to connect patients with interpreters and translated materials.
It’s possible. It’s proven. It’s necessary.
Frequently Asked Questions
Can I be denied an interpreter at a hospital or pharmacy?
No. By federal law, any healthcare provider that receives federal funding-including Medicare, Medicaid, or grants-must provide free professional interpretation services. You cannot be turned away or asked to pay for an interpreter. If you’re denied, ask for the compliance officer or file a complaint with the Office for Civil Rights.
Are family members ever okay to interpret for medication instructions?
Only in emergencies. For anything involving dosage, timing, side effects, or interactions, never rely on family. Studies show up to 25% of interpretations by untrained people contain dangerous errors. A child might not know what hypotension means. A cousin might mishear twice daily as once daily. Professional interpreters are trained in medical terms and ethics. They won’t guess. They’ll ask for clarification.
What if my language isn’t commonly spoken here?
Even for less common languages, most hospitals and large pharmacies have access to remote video or phone interpreters with 200+ language options. If they say they can’t help, ask them to call their language service provider directly. Many services like LanguageLine Solutions offer 24/7 access to interpreters for over 200 languages. You have the right to that service.
Can I get my prescription labels translated?
Yes. You can ask the pharmacy to print your label in your language. Many now offer this for common languages like Spanish, Mandarin, Vietnamese, and Arabic. If they say they can’t, ask them to write out the instructions by hand in your language. They’re required to ensure you understand your medication-even if they have to do it manually.
What’s the teach-back method, and how do I use it?
Teach-back is when you ask the patient to explain the instructions back in their own words. Say: “Can you show me how you’ll take this pill?” or “What will you do if you feel dizzy after taking this?” If they can’t explain it correctly, the provider needs to try again. It’s not about testing you-it’s about making sure you’re safe. Use it every time you get a new prescription.


Gregory Rodriguez
February 4, 2026 AT 13:06Elliot Alejo
February 6, 2026 AT 02:30lance black
February 8, 2026 AT 00:45Jennifer Aronson
February 8, 2026 AT 00:57Pamela Power
February 9, 2026 AT 12:05Gregory Rodriguez
February 10, 2026 AT 20:42Johanna Pan
February 10, 2026 AT 22:59anjar maike
February 12, 2026 AT 22:52Kate Gile
February 12, 2026 AT 23:56Sam Salameh
February 13, 2026 AT 07:41Jenna Elliott
February 13, 2026 AT 11:49