Medication Recalls: What Patients Should Do Immediately
 Feb, 13 2026
Feb, 13 2026
If your doctor prescribed a medication and suddenly you hear it’s being recalled, your first thought might be to stop taking it right away. But that’s exactly what you shouldn’t do - at least not without talking to someone first. Medication recalls are more common than most people realize, and panic can do more harm than good. In 2022 alone, nearly 5,000 drug recalls were issued in the U.S., and while some sound scary, the vast majority aren’t life-threatening. The real danger? Stopping your medicine without a plan.
What a Medication Recall Actually Means
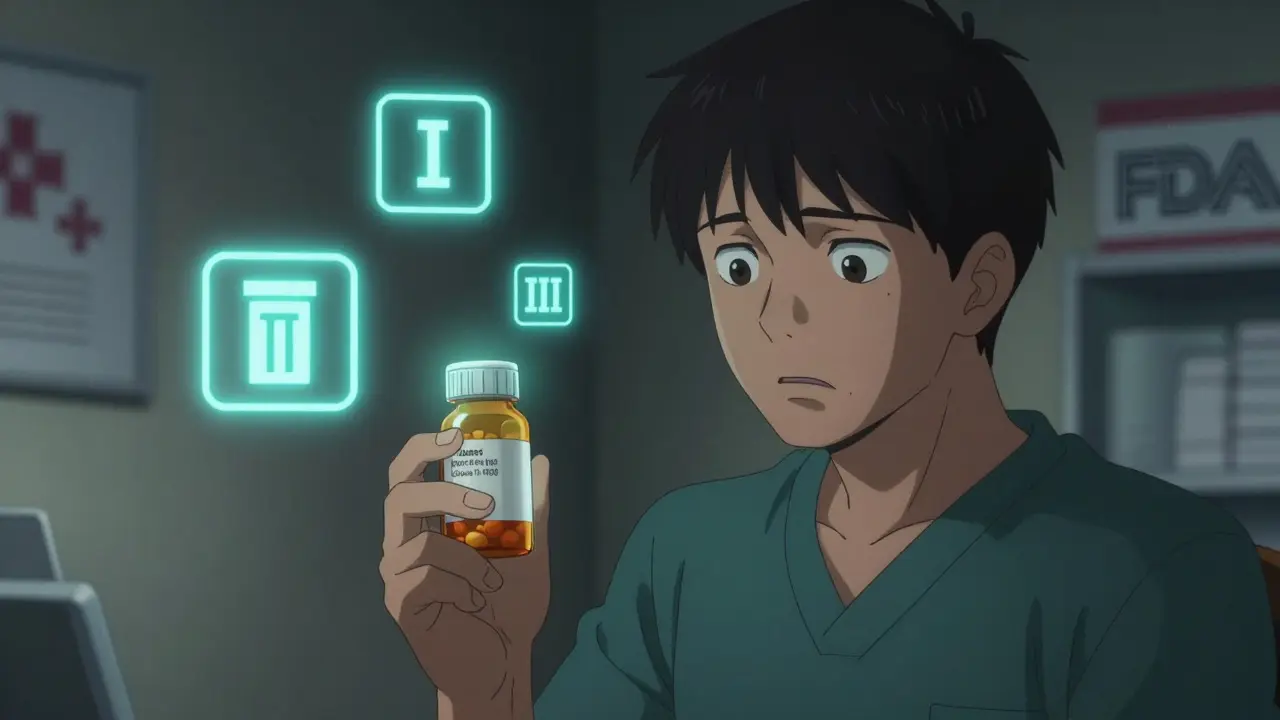
A recall doesn’t mean your drug is definitely dangerous. It means something went wrong during manufacturing, labeling, or packaging. Maybe a batch got contaminated. Maybe the label says 10 mg but the pill inside is 20 mg. Or maybe it was stored improperly and lost its strength. The FDA classifies recalls into three levels based on risk:- Class I - highest risk. Could cause serious harm or death. About 15% of recalls fall here.
- Class II - moderate risk. Might cause temporary health problems. Most common.
- Class III - lowest risk. Unlikely to hurt you. Often just labeling errors.
Most recalls - around 65% - happen because of manufacturing mistakes. Only 5% involve life-threatening issues. But even if it’s just a mislabeled bottle, the FDA still acts. Why? Because mistakes can slip through. And if you’re on a blood pressure pill and the dose is wrong? That’s a real problem.
What You Must Do Right Now
Don’t wait. Don’t scroll through social media. Don’t assume your bottle is safe just because it looks fine. Here’s what to do in order:- Check your lot number and expiration date. Every recall notice includes exact lot numbers. Your pill bottle or box will have a code like “AB12345” or “NDC 00789-123-45.” Compare it to the FDA’s recall list. Don’t guess. Don’t rely on the brand name alone - different manufacturers make the same drug, and only one batch might be affected.
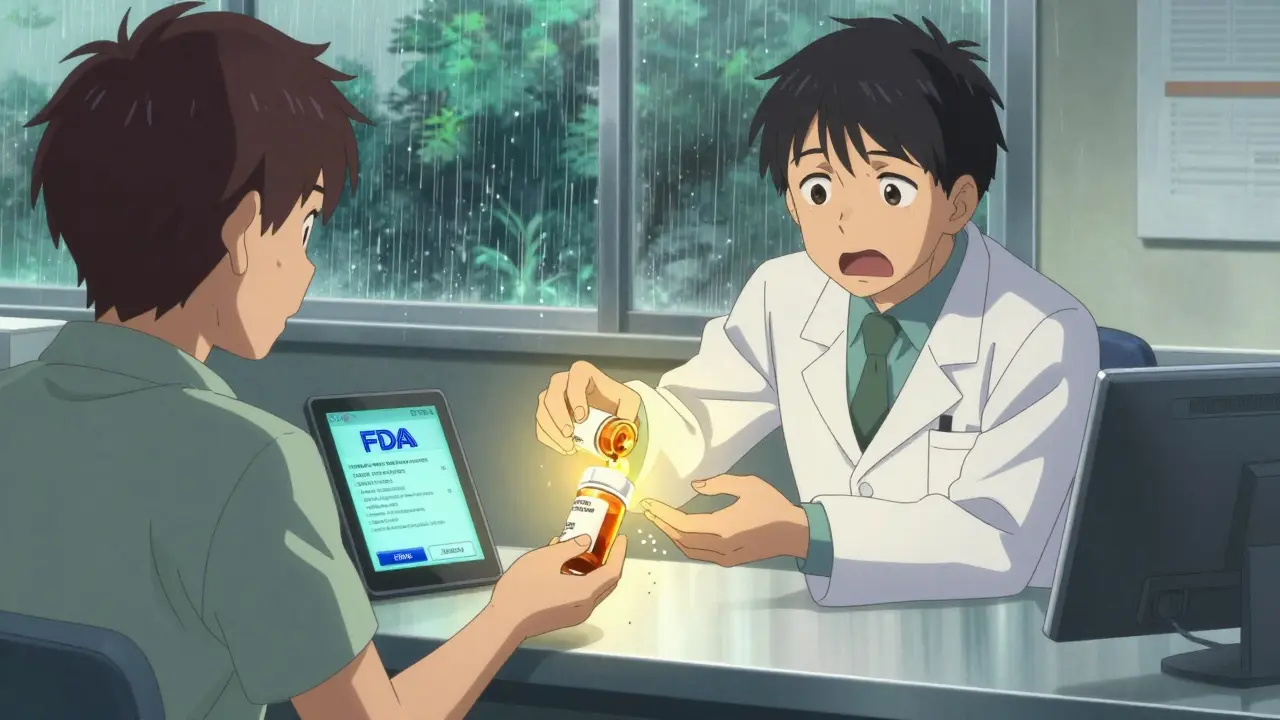
- Call your pharmacy. Pharmacists are your first line of defense. They get recall alerts the same minute the FDA releases them. They can check if your exact bottle is affected. Most pharmacies have a 24- to 48-hour replacement system ready. They’ll give you a new bottle from a clean batch or switch you to another brand - no extra cost.
- Do NOT stop taking your medicine. This is the biggest mistake patients make. In 2022, the FDA found that 22% of people stopped their meds immediately after a recall. For someone with high blood pressure, diabetes, or epilepsy, stopping cold turkey can cause seizures, strokes, or heart attacks. The FDA’s own guidance says: “Continue taking your medicine until your doctor or pharmacist tells you what to do.”
- Look up the recall on the FDA website. Go to fda.gov/recalls. Search by your drug’s brand name or active ingredient. Use the “Product Type” filter to narrow results. Click on the recall notice. It will tell you exactly which lot numbers are affected, why it was recalled, and what to do next.
What to Do If Your Medicine Is Recalled
If your lot number matches the recall, your pharmacy will help you get a replacement. But if you can’t reach them right away - or if you’re worried about side effects from the recalled batch - here’s what to watch for:- Track your symptoms. Did you feel dizzy, nauseous, or unusually tired after taking the pill? Keep a simple log: date, time, dose, and how you felt. This helps your doctor decide if you need a different treatment.
- Dispose of it properly. If you’re told to throw it away, don’t flush it or toss it in the regular trash. Mix the pills with something unappetizing - used coffee grounds, cat litter, or dirt. Seal it in a plastic bag. That stops kids or pets from digging through the trash. The FDA says this is the safest way to dispose of recalled meds.
- Report bad reactions. If you think the recalled drug made you sick, report it. The FDA’s MedWatch program lets patients file reports directly. In 2022, 27% of new recalls started because of patient reports. Your input saves lives.
Common Mistakes (And How to Avoid Them)
Most people make the same three errors during a recall:- Mistake #1: Assuming all versions of the drug are affected. Only one lot number is bad. Your bottle might be fine. Always check the code.
- Mistake #2: Throwing pills in the toilet or trash. That’s dangerous for the environment and for curious kids. Always mix and seal.
- Mistake #3: Waiting to call your pharmacist. Don’t wait a day. Call today. Pharmacies have systems in place. They’re ready.
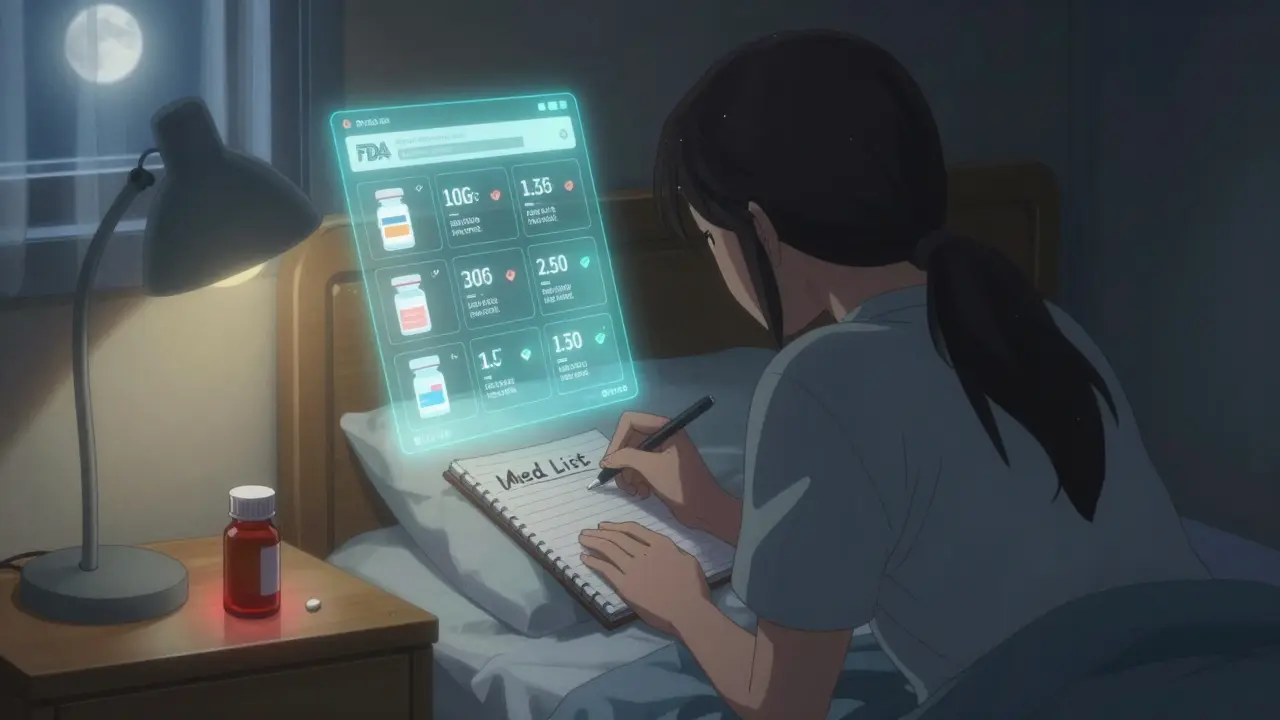
And here’s one more thing: keep a simple list of all your meds - brand name, dose, lot number, expiration date. Update it every time you refill. According to a 2023 survey, patients who do this resolve recall issues 60% faster. That’s not luck. That’s preparation.
Why This Matters Right Now
Recalls are rising. From 2021 to 2022, there was a 12% jump in drug recalls. Blood pressure medications (like valsartan) and diabetes drugs made up nearly one-third of all Class I recalls. Why? Manufacturing shortcuts, supply chain stress, and global sourcing. The FDA is trying to fix this with faster digital alerts. By 2024, pharmacies and insurers will start sending recall texts directly to patients. But until then, you’re your own best defense.Don’t wait for a letter. Don’t rely on news alerts. If you take any prescription, check your bottles now. Look at the lot number. Know your pharmacy’s recall process. Keep your meds list updated. The system works - but only if you act.
Should I stop taking my medication if it’s recalled?
No, not unless your pharmacist or doctor tells you to. Stopping your medicine suddenly can be dangerous, especially for conditions like high blood pressure, diabetes, or heart disease. The FDA specifically advises continuing your current dose until you get a safe replacement. The recall doesn’t mean the drug is toxic - it means there’s a manufacturing issue that needs fixing. Your healthcare provider will guide you on what to do next.
How do I find out if my medication is recalled?
Check the FDA’s official recall page at fda.gov/recalls. Search by your drug’s brand name or active ingredient. Then, compare the lot number on your bottle to the one listed in the recall notice. You can also call your pharmacy - they’re notified immediately and can confirm whether your specific bottle is affected. Don’t rely on news headlines or social media posts; they’re often inaccurate or incomplete.
What if I already took a recalled pill?
If you’ve taken one or two doses from a recalled batch, the risk is usually low - especially for Class II or III recalls. But if you’re concerned, contact your pharmacist or doctor. They can assess your situation based on the drug, the reason for the recall, and your health history. If you notice new symptoms like dizziness, nausea, or unusual fatigue, write them down and share them with your provider. The FDA’s Adverse Event Reporting System (FAERS) tracks these reports, and your input helps improve drug safety.
Can I return the recalled medication to the pharmacy?
Yes. Most pharmacies will accept recalled medication for safe disposal and replace it with a new, unaffected batch at no cost. Some may ask you to bring the original bottle and prescription label. Don’t throw it away yourself unless instructed to - pharmacists know how to dispose of it properly. If your pharmacy is out of stock, they’ll order a replacement from another manufacturer or source within 48 hours.
Why do recalls happen so often?
Most recalls - about 65% - happen because of manufacturing problems: pills with the wrong dose, contamination during production, or packaging errors. Global supply chains mean drugs are made in multiple countries, and even small mistakes can trigger a recall. The FDA doesn’t wait to act - they act as soon as a problem is found. That’s actually a sign the system is working. The goal isn’t to scare you - it’s to catch issues before they hurt people.


Daniel Dover
February 13, 2026 AT 18:09Josiah Demara
February 14, 2026 AT 22:05Chiruvella Pardha Krishna
February 16, 2026 AT 03:45Esha Pathak
February 16, 2026 AT 20:37Joe Grushkin
February 18, 2026 AT 14:32Virginia Kimball
February 20, 2026 AT 09:12Mandeep Singh
February 22, 2026 AT 02:53Michael Page
February 23, 2026 AT 06:20Betty Kirby
February 23, 2026 AT 12:18Kaye Alcaraz
February 23, 2026 AT 20:04