Meniere’s Diet: How Sodium Restriction and Fluid Balance Reduce Vertigo and Hearing Loss
 Jan, 29 2026
Jan, 29 2026
If you have Meniere’s disease, you’ve probably heard that cutting back on salt might help. But why? And how much is really enough? It’s not just about avoiding the salt shaker. It’s about retraining how your body handles fluid - especially in your inner ear.
What’s Really Going On in Your Inner Ear?
Meniere’s disease isn’t just dizziness or ringing in the ears. It’s a buildup of fluid called endolymph in the inner ear. That fluid pressure messes with your balance and hearing signals, causing those sudden vertigo attacks, muffled hearing, and the feeling that your ear is stuffed with cotton. The exact cause isn’t known, but one thing is clear: too much sodium makes this fluid buildup worse.Sodium pulls water into your bloodstream and, eventually, into your inner ear. When your body holds onto extra fluid because of high salt intake, the delicate balance in your cochlea and vestibular system gets thrown off. That’s why doctors have been telling people with Meniere’s to go low-sodium since the 1920s - and why the advice hasn’t changed.
How Much Sodium Is Too Much?
The numbers might surprise you. Most health guidelines say adults should aim for under 2,300 mg of sodium per day. But for Meniere’s, that’s not enough. The real target? Between 1,500 and 2,000 mg per day. That’s about three-quarters of a teaspoon of table salt - and most of it isn’t even coming from your salt shaker.A 2024 study in Acta Otolaryngologica followed 50 people with moderate to severe Meniere’s who cut their sodium to exactly 1,500 mg per day and drank 35 ml of water per kilogram of body weight daily. After six months, their hearing improved by an average of 12.3 dB on audiometry tests. Vertigo attacks dropped in frequency. Tinnitus got quieter. Dizziness scores fell nearly in half. These weren’t minor changes. These were measurable, clinical improvements.
Some experts, like Dr. Richard Miyashita from Tokyo Medical University, argue that sodium restriction works because it boosts aldosterone - a hormone that helps your body manage salt and water balance. When sodium drops, aldosterone rises, helping your inner ear drain excess fluid. Other researchers think it’s more about reducing overall fluid pressure. Either way, the result is the same: less pressure in the ear = fewer symptoms.
It’s Not Just Salt - It’s Hidden Sodium
You might think you’re eating clean. But 77% of the sodium in the average diet comes from packaged, processed, and restaurant food. That means even if you never add salt to your meals, you could still be hitting 3,000 mg a day without realizing it.Here’s where people get tripped up:
- One tablespoon of soy sauce = 900 mg sodium
- A single slice of processed cheese = 400 mg
- A cup of canned soup = 800-1,200 mg
- Even “healthy” granola bars can have 150-300 mg per serving
Read labels. Always. Look for “sodium” on the nutrition facts. If a food has more than 400 mg per serving, it’s probably not a good fit. Choose “low sodium” or “no salt added” versions. When you’re out to eat, ask for food to be cooked without salt. Most kitchens will accommodate you - especially if you explain it’s for a medical condition.
Fluid Balance: Drink More Water? Really?
You might think, “If sodium causes fluid buildup, shouldn’t I drink less?” Actually, no. Dehydration makes your body hang onto even more water - including in your inner ear. The goal isn’t to restrict water. It’s to balance it.The 2024 study used a precise amount: 35 milliliters of water per kilogram of body weight. For a 70 kg (154 lb) person, that’s about 2.5 liters per day. Spread it out. Don’t chug it all at once. Sip steadily. Keep a water bottle handy. If you’re drinking enough, your urine should be pale yellow.
Why does this work? Consistent hydration tells your kidneys to flush out excess sodium instead of storing it. It’s like keeping your plumbing clear - you don’t turn off the water; you keep it flowing smoothly.
What Else Should You Avoid?
Sodium and water aren’t the whole story. Caffeine and alcohol are also troublemakers.Caffeine - in coffee, tea, soda, and chocolate - narrows blood vessels. That includes the tiny ones feeding your inner ear. Less blood flow means less oxygen and more pressure buildup. Many patients report fewer vertigo attacks after cutting out morning coffee or switching to decaf.
Alcohol is even trickier. It dehydrates you, disrupts your balance system, and can trigger attacks hours after you’ve had a drink. One glass of wine might not seem like much, but for someone with Meniere’s, it can be enough to set off a 24-hour spiral of dizziness and ear pressure.
Some people also find that sugar spikes worsen symptoms. While the science isn’t as strong here, many patients report better control when they reduce refined carbs and sweets. It’s worth experimenting with - especially if you’re already cutting out processed foods.
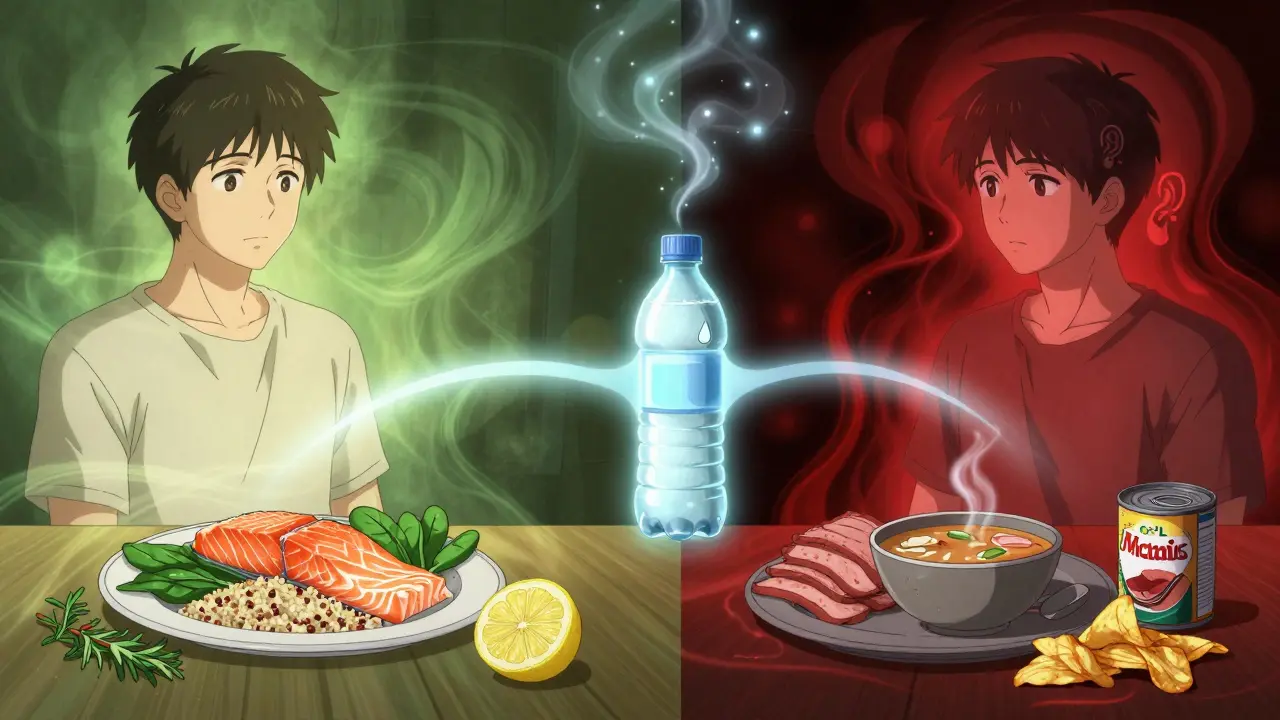
What Can You Actually Eat?
A low-sodium Meniere’s diet isn’t about deprivation. It’s about rediscovering real food.- Fresh vegetables and fruits - naturally low in sodium, high in potassium (which helps balance sodium)
- Lean meats and poultry - buy unprocessed, skinless, and cook without salt
- Fresh or frozen fish - avoid smoked or canned varieties unless labeled “no salt added”
- Whole grains - brown rice, quinoa, oats - check labels for added sodium
- Legumes - beans and lentils, rinsed well if canned
- Herbs and spices - garlic, ginger, lemon juice, black pepper, cumin, paprika - use them generously
Snacks? Try plain nuts, unsalted popcorn, apple slices with almond butter, or hummus made from scratch. Avoid pretzels, chips, crackers, and deli meats - even the “low-fat” ones are loaded with salt.
Why Diet Beats Pills - and When Pills Might Still Be Needed
Diuretics like hydrochlorothiazide are often prescribed to flush out fluid. They can help - but they come with side effects: dizziness, low potassium, kidney stones, and dehydration. And they don’t fix the root problem. They just mask it.Dietary changes? No side effects. No prescriptions. Just your body learning to balance itself again. One study found that 68% of patients saw major improvement with sodium restriction alone - without any medication.
But diet isn’t magic. If your symptoms are severe and don’t improve after 3-6 months of strict eating, your doctor might suggest other options: steroid injections into the ear (which reduce inflammation) or gentamicin injections (which disable the balance part of the inner ear to stop vertigo). These are serious procedures with risks - and they’re only considered after diet and medication have been tried.
Sticking With It: The Real Challenge
The hardest part isn’t knowing what to eat. It’s doing it every day, in every situation.Family dinners. Work lunches. Travel. Holidays. Social events. It’s easy to say, “I’ll start Monday.” But Meniere’s doesn’t wait.
Start small. Swap one high-sodium item per week. Learn to read labels. Keep a food journal for two weeks - you’ll be shocked at how much sodium you’re eating without realizing it.
And don’t beat yourself up if you slip. One salty meal won’t ruin your progress. But if you go back to eating like you used to, your symptoms will come back.
Many people report that after 4-6 weeks, food starts tasting better. Your taste buds reset. You notice the natural sweetness in carrots, the earthiness in mushrooms, the brightness in lemon. You don’t miss the salt - you start appreciating the food more.
What’s Next?
The National Institutes of Health is currently running a major study called the Meniere’s Dietary Intervention Trial (NCT04567891). They’re comparing 1,500 mg versus 2,300 mg of sodium per day over 12 months, with results expected in late 2025. This could finally give us the high-quality evidence we’ve been waiting for.In the meantime, the evidence we have is strong enough. Low-sodium, well-hydrated eating isn’t a fad. It’s the most effective, safest, and most accessible tool we have to take control of Meniere’s disease - without drugs, without surgery, without side effects.
You don’t need to be perfect. But you do need to be consistent. Your ears will thank you.
Can I still eat out if I have Meniere’s disease?
Yes - but you need to be strategic. Ask for food to be prepared without added salt. Avoid sauces, soups, and dressings unless they’re labeled low-sodium. Choose grilled or steamed proteins, plain vegetables, and brown rice. Skip appetizers like chips, pretzels, or bread baskets. Most restaurants will accommodate you if you explain you’re managing a medical condition.
How long does it take to see results from a low-sodium diet?
Most people notice small improvements in ear pressure and dizziness within 2-4 weeks. Significant changes in vertigo frequency and hearing usually take 3-6 months. The 2024 study showed clear improvements at the 6-month mark. Consistency matters more than perfection.
Is it okay to use salt substitutes like potassium chloride?
Some people use potassium-based salt substitutes, but talk to your doctor first. If you have kidney problems or take certain medications like ACE inhibitors or spironolactone, too much potassium can be dangerous. Natural flavor boosters like lemon, herbs, and spices are safer alternatives.
Does caffeine really make Meniere’s worse?
Yes - for many people. Caffeine constricts blood vessels, including those in the inner ear. This can reduce blood flow and worsen fluid buildup. Cutting back on coffee, energy drinks, and even dark chocolate often leads to fewer attacks. Try switching to herbal teas or decaf.
Can I drink alcohol occasionally?
It’s risky. Alcohol dehydrates you and directly affects the vestibular system. Even one drink can trigger vertigo hours later. Many patients find they need to avoid it completely. If you do drink, limit it to a small glass of wine and drink extra water afterward - but be prepared for possible symptoms the next day.
Do I need to take supplements on a low-sodium diet?
Not usually. A diet rich in fresh fruits, vegetables, whole grains, and lean proteins provides all the nutrients you need. Potassium helps balance sodium, so foods like bananas, spinach, sweet potatoes, and avocados are helpful. Avoid potassium supplements unless your doctor recommends them.
Meniere’s disease doesn’t have a cure - but it does have a manageable path. By focusing on sodium, water, and real food, you’re not just treating symptoms. You’re giving your inner ear the environment it needs to heal.


Laia Freeman
January 29, 2026 AT 20:16kabir das
January 30, 2026 AT 03:12Keith Oliver
January 31, 2026 AT 00:35Kacey Yates
January 31, 2026 AT 00:42ryan Sifontes
January 31, 2026 AT 04:55Laura Arnal
February 1, 2026 AT 12:16Jasneet Minhas
February 2, 2026 AT 05:26Eli In
February 3, 2026 AT 20:55Megan Brooks
February 5, 2026 AT 05:53Ryan Pagan
February 7, 2026 AT 01:50Robin Keith
February 8, 2026 AT 21:33Sheryl Dhlamini
February 9, 2026 AT 06:41LOUIS YOUANES
February 9, 2026 AT 13:07Andy Steenberge
February 11, 2026 AT 09:04