Safe Use of Multiple Medications: Avoiding Double Ingredients
 Feb, 21 2026
Feb, 21 2026
Every year, tens of thousands of people end up in emergency rooms because they took too much of the same medicine - not because they meant to, but because they didn’t realize they were taking it twice. This isn’t a rare mistake. It’s one of the most common, preventable medication errors out there. And it’s happening to people who are doing everything right: taking their prescriptions, reading labels, following their doctor’s advice. The problem? Double ingredients.
What Exactly Are Double Ingredients?
Double ingredients happen when you take two or more medications that contain the same active ingredient. It’s not about drug interactions between different chemicals - it’s about the same chemical showing up under different names. Think of it like this: you take a prescription painkiller for your back, and then you grab a store-brand cold tablet because you’ve got a stuffy nose. Both contain acetaminophen. You don’t know it. Your body gets hit with twice the dose. And that’s enough to damage your liver. The most common culprit? Acetaminophen. It’s in over 600 different products - from pain relievers like Tylenol to cold and flu remedies, sleep aids, and even some prescription opioids like Vicodin and Percocet. The National Institutes of Health says more than 56,000 emergency room visits each year in the U.S. are due to accidental acetaminophen overdose. Most of those cases involve people who didn’t realize they were doubling up. Other dangerous overlaps include:- Diphenhydramine - found in Benadryl, NyQuil, ZzzQuil, and many sleep aids. Mixing it with prescription sedatives can cause extreme drowsiness, confusion, or even breathing problems.
- Pseudoephedrine - in Sudafed, Claritin-D, and many cold medicines. Too much can spike your blood pressure and heart rate.
- NSAIDs - like ibuprofen and naproxen - in Advil, Aleve, and some prescription painkillers. Taking multiple can lead to stomach bleeding or kidney damage.
Who’s Most at Risk?
Older adults are hit hardest. People over 65 make up 65% of hospitalizations from double ingredient errors, according to the CDC. Why? Because they’re more likely to have multiple chronic conditions - arthritis, diabetes, high blood pressure - and each condition brings its own medication. Add in OTC products for sleep, pain, or colds, and you’ve got a perfect storm. But it’s not just seniors. Anyone taking five or more medications - whether prescription, OTC, or supplements - is at higher risk. Studies show that 32% of people on five or more drugs have accidentally taken duplicate ingredients at least once. And here’s the kicker: 45% of prescription labels don’t clearly warn you if the medicine shares an ingredient with common OTC products. Even worse? Many people don’t tell their doctors about the OTC stuff they’re taking. They think it’s “just a pill” or “not real medicine.” But if you’re taking NyQuil every night for sleep, that’s a medication. And if you’re also on a prescription antihistamine or sleep aid, you’re doubling up.Why This Keeps Happening
The system isn’t designed to catch this. Doctors focus on one condition at a time. A cardiologist prescribes your blood pressure med. A rheumatologist adds your arthritis pill. A sleep specialist gives you a sedative. Meanwhile, you’re buying cold medicine at the pharmacy without telling anyone. None of them see the full picture. Pharmacies help - but only if you use one. If you fill prescriptions at three different stores, your medication history gets split. One pharmacy can’t see what another has dispensed. A 2021 JAMA study found that using a single pharmacy reduces double ingredient errors by 63%. Electronic health records are supposed to help too. But most systems don’t track OTC meds. They might know you’re on lisinopril and metformin - but not that you’re taking Advil Cold & Sinus every morning. That means alerts for drug interactions often miss the most common danger: duplicate ingredients.
How to Protect Yourself
The good news? Almost 9 out of 10 of these errors can be prevented with simple steps. You don’t need a medical degree. You just need to be proactive.1. Keep a Real, Updated List
Write down everything you take - every day. Not just prescriptions. Include:- All OTC medicines (pain relievers, cold pills, sleep aids)
- Vitamins and supplements
- Herbal remedies and traditional medicines
- Dosage and how often you take each one
- Why you take it (e.g., “for headaches,” “for sleep”)
2. Use One Pharmacy
Fill all your prescriptions at the same pharmacy. Pharmacists have systems that flag duplicate ingredients. They’re trained to spot this. And when you use one pharmacy, they can see everything you’re getting - even if it’s not a prescription. A 2021 study showed this cuts double ingredient errors by over 60%.3. Ask the Right Questions
When a doctor or pharmacist gives you a new medicine, ask:- “What’s the active ingredient?”
- “Is this the same as anything else I’m taking?”
- “Could this be in a cold medicine or painkiller I already have?”
4. Read the Drug Facts Label
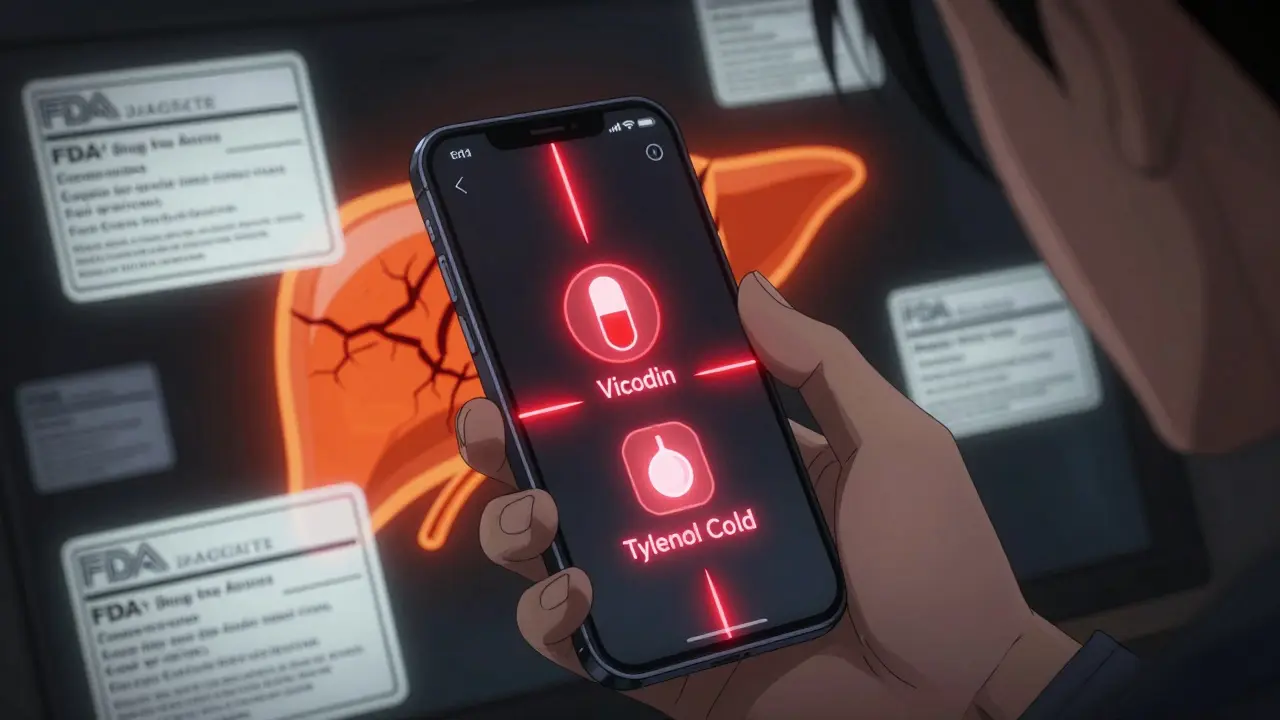
Since 2020, the FDA requires all OTC medicines to have a standardized “Drug Facts” label. It’s designed to make active ingredients easy to find. Look for the section labeled “Active Ingredients.” If you see the same name twice - even if the brand names are different - you’re doubling up. For example:- Prescription: Vicodin → Active ingredient: acetaminophen + hydrocodone
- OTC: Tylenol Cold → Active ingredient: acetaminophen + phenylephrine
5. Review Your Meds Once a Year
Ask your primary care provider to do a full medication review. This isn’t a one-time thing. It should happen every year. Bring your list. Ask: “Are all these still necessary? Could any be causing hidden overlaps?”What to Do If You Think You’ve Overdosed
Symptoms of double ingredient overdose vary by ingredient:- Acetaminophen: Nausea, vomiting, stomach pain, loss of appetite, jaundice (yellow skin/eyes)
- Diphenhydramine: Extreme drowsiness, confusion, trouble urinating, fast heartbeat
- Pseudoephedrine: High blood pressure, severe headache, rapid heartbeat, chest pain
- NSAIDs: Black or bloody stools, vomiting blood, swelling in legs, reduced urination
What’s Being Done to Fix This
The system is slowly catching up. The American Geriatrics Society updated its Beers Criteria in 2023 to flag 15 high-risk double ingredient combinations. The FDA’s new labeling rules (required by 2025) will make active ingredients even clearer. Apple Health and other apps now flag duplicate ingredients on iPhones. And 87% of U.S. healthcare systems now have tools to check for these errors - though only 43% track OTC meds properly. But none of that matters if you don’t take control yourself. Technology helps - but your list, your questions, and your honesty with your providers are the real shields.Final Thought: You’re the Best Medication Detective
No one else will know your full medicine routine like you do. Doctors see you for 15 minutes. Pharmacists see one prescription at a time. But you live with your pills every day. You’re the only one who can connect the dots. Start today. Write down every pill, drop, and patch. Keep it updated. Use one pharmacy. Ask the questions. You don’t need to be an expert. Just be informed. Because when it comes to double ingredients, knowledge isn’t just power - it’s your liver, your brain, and maybe your life.Can I take OTC painkillers if I’m already on a prescription painkiller?
Only if you know exactly what’s in both. Many prescription painkillers, like Vicodin or Percocet, already contain acetaminophen. Taking Advil or Tylenol on top of that can lead to liver damage. Always check the active ingredients on both labels before adding any OTC pain reliever.
I use multiple pharmacies. Should I switch to just one?
Yes. Using a single pharmacy allows pharmacists to see your full medication history, including OTC products. This helps them flag dangerous overlaps before you take them. Studies show this reduces double ingredient errors by over 60%. If you can’t switch, at least keep a detailed list and bring it to every pharmacy.
Do supplements count as medications?
Yes. Many herbal supplements contain active ingredients that can overlap with prescription or OTC drugs. For example, valerian root and melatonin both cause drowsiness - mixing them with prescription sleep aids can be dangerous. Always list supplements on your medication list and mention them to your pharmacist.
Why don’t doctors ask about OTC medicines?
Many doctors assume patients only take prescriptions. They’re not trained to routinely ask about OTC use. But 49% of double ingredient cases happen when people take multiple OTC products together. Always volunteer this information. Say: “Here’s what I’m taking on my own - can you check for risks?”
How can I tell if two medicines have the same ingredient?
Look at the “Active Ingredients” section on the Drug Facts label - it’s required by the FDA to be clearly listed. Don’t rely on brand names. For example, “acetaminophen” is the same as “paracetamol” (used outside the U.S.). If both medicines list the same active ingredient, you’re doubling up.

