St. John’s Wort and Prescription Drugs: What You Need to Know Before Taking It
 Dec, 24 2025
Dec, 24 2025
St. John’s Wort isn’t just another herbal supplement. For many people, it’s the go-to remedy for mild depression-especially those tired of prescription side effects like weight gain, low libido, or brain fog. But here’s the catch: St. John’s Wort doesn’t play nice with most prescription drugs. And if you’re taking anything from birth control to heart medication, this one mistake could put your health at serious risk.
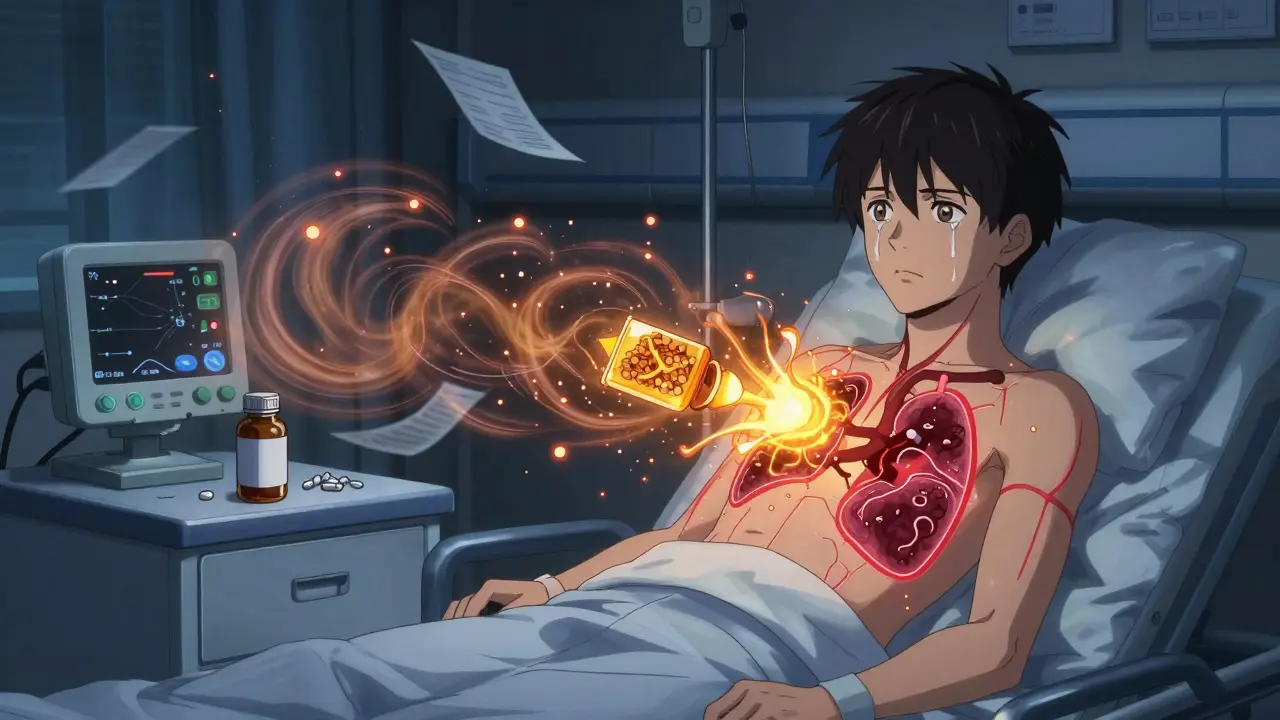
How St. John’s Wort Changes How Your Body Handles Medications
St. John’s Wort works by flipping a switch in your liver called the pregnane-X-receptor, or PXR. When this switch turns on, your body starts making more of certain enzymes-mainly CYP3A4, CYP2C9, and CYP1A2-that break down drugs. Think of it like your liver suddenly going into overdrive, cleaning out medications before they have time to do their job.
This isn’t theoretical. In 2019, a 34-year-old woman in the U.S. had a kidney transplant and was stable on tacrolimus, a drug that keeps her body from rejecting the new organ. Then she started taking St. John’s Wort for low mood. Eight weeks later, her tacrolimus levels dropped by over 60%. Her body rejected the transplant. She ended up back in the hospital. This isn’t rare. Similar cases have happened with heart, liver, and lung transplant patients.
The active ingredient behind this? Hyperforin. It’s in most commercial St. John’s Wort extracts-usually 2% to 5%. Even a daily dose of 300 mg can trigger this reaction. And here’s the kicker: it takes about 10 days for your body to fully ramp up these enzymes. So you might feel fine at first. Then, out of nowhere, your medication stops working.
The Medications That Can Become Ineffective (or Dangerous)
St. John’s Wort doesn’t just reduce effectiveness-it can turn safe drugs into dangerous ones. Here are the big ones:
- Immunosuppressants like cyclosporine, tacrolimus, and sirolimus: Used after organ transplants. If St. John’s Wort lowers their levels, your body attacks the new organ. Death risk: real.
- Antiretrovirals for HIV: Drugs like protease inhibitors (e.g., indinavir, ritonavir) can drop to half their level. That means the virus comes back, resistance builds, and treatment fails.
- Oral contraceptives: Birth control pills, patches, rings. Studies show women on St. John’s Wort have higher rates of unintended pregnancy. One study found 1 in 5 women experienced breakthrough bleeding or ovulation. That’s not a side effect-it’s a failure.
- Anticoagulants like warfarin: INR levels (which measure blood thinning) can plummet. One documented case saw INR drop from 2.5 to 1.4 in 10 days. That’s the difference between safe and a stroke or internal bleed.
- Antidepressants like SSRIs and SNRIs: Taking St. John’s Wort with Prozac, Zoloft, or Effexor can cause serotonin syndrome. Symptoms? Agitation, rapid heart rate, high fever, seizures. It’s rare, but it’s deadly.
- Pain meds like oxycodone, methadone, tramadol: These rely on CYP3A4 to work. St. John’s Wort can make them useless. People report sudden, unexplained pain returning after starting the herb.
- Statins like atorvastatin: Cholesterol meds may lose potency. That means your LDL stays high, and your heart risk climbs.
There are over 50 documented interactions. The European Medicines Agency says St. John’s Wort should never be used with drugs that have a narrow therapeutic index-meaning the difference between a helpful dose and a toxic one is tiny. That includes most of the drugs above.
Why People Think It’s Safe-And Why They’re Wrong
Many people assume herbal means harmless. After all, it’s natural. But that’s a dangerous myth. Aspirin is natural too-it comes from willow bark. That doesn’t mean you can take it with blood thinners without risk.
St. John’s Wort is also sold as a supplement. In the U.S., the FDA doesn’t approve supplements before they hit the shelf. Labels often say “may interact with medications” in tiny print. But in Germany, where it’s prescribed like a drug, labels list exact interactions: “Do not use with oral contraceptives, cyclosporine, or antiretrovirals.” That’s the difference between a warning and a red flag.
And then there’s the placebo effect. People feel better on St. John’s Wort because they believe it works. But if they’re also on a medication that’s now being broken down too fast, they’re not getting the benefit of either. One Reddit user wrote: “I took St. John’s Wort for anxiety and felt great-until I realized my blood pressure meds weren’t working anymore.”
Who Should Never Take It
St. John’s Wort isn’t for everyone. Avoid it completely if you:
- Have had an organ transplant
- Are on HIV medication
- Take birth control pills or use hormonal IUDs
- Are on warfarin, rivaroxaban, or other blood thinners
- Take any antidepressant (SSRI, SNRI, MAOI)
- Use opioids for chronic pain
- Are over 65 and taking multiple medications
Even if you’re not on any of these now, you might be soon. A 2022 study found that 38% of people who started St. John’s Wort for depression began taking a new prescription within six months. That’s a ticking time bomb.
What to Do Instead
If you’re looking for a natural alternative to treat mild depression, here are safer options:
- SAM-e: Works for mood with minimal drug interactions. Only known risk is with MAO inhibitors-rarely used today.
- 5-HTP: A precursor to serotonin. Fewer interactions than St. John’s Wort, but still use caution with antidepressants.
- Exercise: A 2020 meta-analysis showed regular walking or cycling was as effective as SSRIs for mild depression.
- Cognitive behavioral therapy (CBT): Free or low-cost apps like Woebot or Moodfit have proven results.
- Vitamin D: Low levels are linked to depression. Getting your levels checked and supplementing if needed can help.
None of these have the same level of evidence as St. John’s Wort-but they also don’t risk your life-saving medications.
What to Do If You’re Already Taking It
If you’re on St. John’s Wort and any prescription drug, don’t stop cold turkey. Talk to your pharmacist first. They’re trained to spot these interactions.
Here’s what to do:
- Make a list of every medication, supplement, and herb you take-including over-the-counter stuff.
- Go to a pharmacy and ask for a drug interaction check. Most offer it for free.
- If you’re on a critical drug like cyclosporine or warfarin, get a blood test to check levels before and after stopping St. John’s Wort.
- Wait at least two weeks after stopping St. John’s Wort before starting a new medication. The enzyme induction doesn’t stop right away.
- Don’t switch to another herb without professional advice. Many have hidden interactions too.
One woman in Sydney stopped St. John’s Wort after her doctor found her INR had dropped to 1.2. She was on warfarin for a history of clots. Within three weeks of stopping the herb and adjusting her dose, her INR stabilized at 2.3. She didn’t have a stroke. She didn’t bleed out. She just got smart.
The Bottom Line
St. John’s Wort might help your mood. But if you’re on any prescription drug, it’s not worth the risk. The consequences aren’t just side effects-they’re organ rejection, unintended pregnancy, stroke, or death. The data is clear. The warnings are loud. And yet, people still take it without telling their doctors.
This isn’t about scaring you. It’s about giving you real facts. Natural doesn’t mean safe. Herbal doesn’t mean harmless. And when it comes to your medications, you don’t get a second chance.
If you’re thinking of trying St. John’s Wort, talk to a pharmacist first. Not your friend. Not your yoga instructor. A licensed professional who knows how drugs work in your body.
There are safer ways to feel better. Use them.
Can St. John’s Wort interact with birth control pills?
Yes. St. John’s Wort can reduce the effectiveness of birth control pills, patches, rings, and even some IUDs by speeding up how fast your body breaks down hormones. Studies show women on St. John’s Wort have higher rates of breakthrough bleeding and unintended pregnancy. If you’re using hormonal birth control, avoid St. John’s Wort completely.
How long does St. John’s Wort stay in your system after you stop taking it?
The enzyme-inducing effects of St. John’s Wort can last up to two weeks after you stop taking it. Even if you feel fine, your liver may still be breaking down medications faster than normal. That’s why doctors recommend waiting at least 14 days before starting or adjusting any prescription drug after stopping St. John’s Wort.
Is St. John’s Wort safe if I’m not on any medications?
If you’re not taking any prescription drugs, over-the-counter meds, or other supplements, St. John’s Wort is generally safe for short-term use in treating mild depression. But even then, side effects like dry mouth, dizziness, or increased sun sensitivity can occur. And if you start any new medication later-even an antibiotic or painkiller-you could trigger an interaction. Always check with a pharmacist before starting any supplement.
Can I take St. John’s Wort with antidepressants?
No. Combining St. John’s Wort with SSRIs, SNRIs, or MAO inhibitors can cause serotonin syndrome-a rare but life-threatening condition. Symptoms include confusion, rapid heartbeat, high fever, muscle rigidity, and seizures. This is not a mild reaction. It requires emergency care. Never mix St. John’s Wort with antidepressants.
Are there any St. John’s Wort products that don’t cause interactions?
Researchers are testing hyperforin-free extracts, which may reduce enzyme induction by up to 90%. But these are not yet widely available to consumers. Even if you find a product labeled “low-hyperforin,” there’s no guarantee it won’t interact. Until these are approved and regulated, assume all St. John’s Wort products carry interaction risks.
Why isn’t St. John’s Wort banned if it’s so dangerous?
In the U.S., herbal supplements aren’t regulated like drugs. The FDA can only act after harm is proven. St. John’s Wort is still sold because it’s classified as a dietary supplement, not a medicine. In Europe, it’s regulated more strictly and requires warning labels. But in the U.S., the burden is on the consumer to know the risks-which many don’t.


Gary Hartung
December 24, 2025 AT 23:31Oh. My. God. I just read this and I’m shaking. I’ve been taking St. John’s Wort for two years-‘natural antidepressant,’ my yoga teacher said. I didn’t even know I was on a blood thinner! My INR was ‘fine’ last month-now I’m sweating bullets. I’m calling my pharmacist tomorrow. I can’t believe I almost killed myself with a bottle from Whole Foods. This is the most terrifying thing I’ve read all year.
Ben Harris
December 25, 2025 AT 01:14So you’re telling me some guy in Germany who got paid to study herbs is more trustworthy than my cousin who swears by St. John’s Wort because she ‘felt lighter’? I mean c’mon. It’s not like the FDA regulates oxygen either. If I want to take a plant and risk my meds that’s my business. You people act like I’m about to inject bleach.
Zabihullah Saleh
December 26, 2025 AT 07:11There’s a deeper cultural fracture here. In the West we treat herbs like toys-free, harmless, ‘wellness.’ In Afghanistan, where I grew up, every leaf has a name, a memory, a warning passed down by grandmothers. We didn’t need FDA studies to know that if you take khat with heart medicine, you don’t wake up. We knew because someone’s uncle died. Now we’ve outsourced wisdom to Amazon reviews. This isn’t about St. John’s Wort-it’s about how we’ve lost the art of listening to elders, to science, to silence.
Winni Victor
December 26, 2025 AT 13:36Ugh. So now I’m supposed to feel guilty for wanting to feel better without being drugged into a zombie? Like, wow. Thanks for the guilt trip, Dr. Doom. I’m on birth control and I take St. John’s Wort and guess what? I’m not pregnant, I’m not dead, and I’m not crying in a bathtub. Your article reads like a horror movie written by a pharmacist with a grudge.
Terry Free
December 27, 2025 AT 22:20Let me get this straight. You’re telling me a supplement that’s been used for centuries is suddenly a death sentence because it ‘induces enzymes’? That’s the same logic that says aspirin is dangerous because it inhibits COX-1. Everything interacts. The real problem? People don’t read labels. Or talk to pharmacists. Or think. This isn’t a crisis-it’s a failure of personal responsibility.
Lindsay Hensel
December 28, 2025 AT 14:59I appreciate the thoroughness of this post. The clinical examples are sobering, especially the transplant case. I urge everyone to treat herbal supplements with the same caution as pharmaceuticals. Your body does not distinguish between ‘natural’ and ‘synthetic’-only between molecules. Please consult a pharmacist before combining any substance with prescribed medication. Your life may depend on it.
Sophie Stallkind
December 28, 2025 AT 18:32Thank you for this. I work in a clinic and see this exact scenario every week. Patients come in saying, ‘I started the herb because my doctor wouldn’t listen.’ But the truth is, most doctors don’t ask about supplements. We need better training. We need pharmacy-led interaction checks built into EHRs. And we need patients to understand: ‘natural’ is not a synonym for ‘safe.’
Katherine Blumhardt
December 29, 2025 AT 02:58Wait so if I stop the st johns wort do i just wait 2 weeks? like literally just sit there? no coffee? no ibuprofen? what if i get a headache??