Sulfonylureas and Weight Gain: What You Need to Know Long-Term
 Oct, 29 2025
Oct, 29 2025
Sulfonylurea Weight Gain Estimator
Estimate potential weight gain when taking sulfonylurea medications based on duration and medication type. This tool uses data from clinical studies and real-world evidence.
Estimated Weight Gain
Calculation Note: Based on clinical studies showing average weight change over time for different sulfonylurea medications. This estimate may vary based on individual factors.
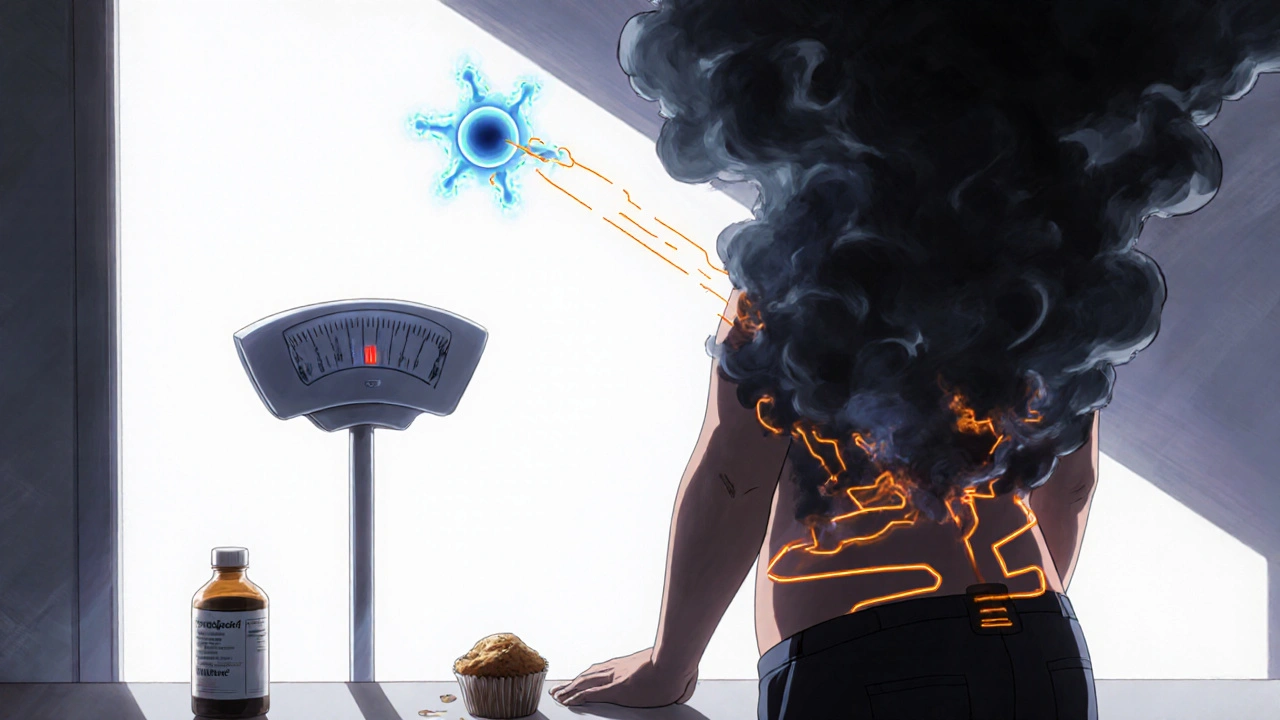
When you’re managing type 2 diabetes, getting your blood sugar under control is the top priority. But what happens when the medicine that helps your glucose also makes you gain weight? For millions of people on sulfonylureas, this isn’t just a side effect-it’s a daily struggle that can undo years of progress.
What Are Sulfonylureas, Really?
Sulfonylureas are one of the oldest oral diabetes drugs still in use today. First introduced in the 1950s, they work by telling your pancreas to pump out more insulin. That insulin then pulls glucose out of your blood and into your cells, lowering your sugar levels. Common brands include glipizide, glyburide, and glimepiride. Gliclazide is another, often overlooked option that behaves differently.
They’re cheap-sometimes as low as $4 a month-and easy to take, usually just once or twice a day. That’s why, even today, they’re prescribed to nearly one in five people with type 2 diabetes in the U.S., especially those on Medicare or without good insurance.
But here’s the catch: your body doesn’t just use that extra insulin to lower blood sugar. It also stores fat.
Why Do Sulfonylureas Make You Gain Weight?
It’s not about eating more. It’s about how your body responds to the extra insulin.
Insulin is a storage hormone. When it’s high, your body says: “Save everything.” Fat cells get the signal to soak up fatty acids. Muscle and liver cells hold onto glucose instead of burning it. Even your appetite can creep up because insulin suppresses the hormone that tells you you’re full.
Studies show that sulfonylureas activate receptors on fat cells that trigger calcium spikes inside them. That calcium jump starts fat production-lipogenesis. In simple terms: more insulin + more fat storage = weight gain.
But not all sulfonylureas are the same. Glimepiride and glyburide are strong insulin stimulators-and they’re linked to the most weight gain. One 2016 study of 51 patients found that 62.7% of those gaining weight were on glimepiride. Meanwhile, gliclazide showed almost no weight gain in the same group. In fact, a 1988 study found people on gliclazide actually lost weight over three years.
How Much Weight Do People Actually Gain?
The numbers vary. Clinical trials say 2-5 kg (4-11 lbs) over the first year. Real-world reports? Often worse.
On the American Diabetes Association’s online forum, 68% of 1,243 users reported weight gain as a “significant problem.” One Reddit user, Type2Warrior87, said he gained 12 pounds in nine months on glipizide-even though he didn’t change his diet or exercise. He switched to metformin and lost it all back in six months.
But here’s the twist: experts disagree. Dr. Ralph A. DeFronzo argues the average gain is only 1.8-2.7 kg over two years in real life, not the 4-5 kg from early trials. Why the difference? Clinical trials often include people who are newly diagnosed and more sensitive to insulin changes. Real patients are often older, heavier, and already insulin resistant-so the effect can be less dramatic, or more unpredictable.
Still, the trend is clear: if you’re on a sulfonylurea and your weight climbs, it’s likely connected.
How Do Sulfonylureas Compare to Other Diabetes Drugs?
Let’s put this in context. Here’s how different diabetes meds affect weight:
| Medication Class | Average Weight Change | Notes |
|---|---|---|
| Sulfonylureas (glimepiride, glyburide) | +2 to +5 kg | Strong insulin stimulation; higher risk with long-term use |
| Sulfonylureas (gliclazide) | +0 to -1 kg | Unique profile-may cause weight loss |
| Metformin | -2 to -3 kg | Weight-neutral or modest loss; first-line choice |
| GLP-1 agonists (semaglutide, liraglutide) | -3 to -7 kg | Reduce appetite, slow digestion; gold standard for weight loss |
| SGLT2 inhibitors (empagliflozin, canagliflozin) | -3 to -6 kg | Make you pee out sugar; lowers blood pressure too |
| Thiazolidinediones (pioglitazone) | +1.5 to +4 kg | Fluid retention and fat storage; rarely used now |
That’s the problem. While newer drugs help you lose weight and protect your heart, sulfonylureas push you in the opposite direction. And weight gain isn’t just about appearance-it raises your risk for high blood pressure, sleep apnea, and even heart disease.
Who Should Avoid Sulfonylureas Because of Weight Gain?
The American Association of Clinical Endocrinologists says: if your BMI is over 35, avoid sulfonylureas. That’s not a random number. At that level, every extra kilogram makes insulin resistance worse. It’s a vicious cycle: more weight → more insulin needed → more insulin → more weight.
Dr. John B. Buse put it bluntly: “Weight gain with sulfonylureas creates a therapeutic paradox.” Your sugar levels might look better on paper, but your body is getting less healthy overall.
And it’s not just about weight. Sulfonylureas also raise your risk of low blood sugar-especially if you skip meals or exercise. That’s dangerous. And the 2015 Diabetes Journals meta-analysis linked them to a 16-55% higher risk of heart problems, possibly because of the weight gain and stress on your pancreas.
What Can You Do If You’re Already on a Sulfonylurea?
You don’t have to quit cold turkey. But you do need a plan.
- Switch to gliclazide. If you’re on glimepiride or glyburide, ask your doctor if gliclazide is an option. It’s just as effective for blood sugar but much gentler on your weight.
- Add metformin. The 2016 Farmacia Journal study showed patients on sulfonylurea + metformin gained 1.2 kg less than those on sulfonylureas alone. Metformin helps your body use insulin better and cuts down on fat storage.
- Move more. The Veterans Affairs Diabetes Trial found that 150 minutes of walking or cycling per week, plus a 500-calorie daily deficit, reduced weight gain by 63%. You don’t need to run a marathon-just be consistent.
- Try time-restricted eating. A 2024 study showed limiting food to an 8-hour window (like 10 a.m. to 6 p.m.) cut sulfonylurea-related weight gain by 78%. Your body gets a break from insulin spikes.
- Track your weight monthly. If you gain more than 3% of your starting weight in six months, it’s time to reconsider your meds.
Why Are Sulfonylureas Still Prescribed?
Because they’re affordable. In a country where a month of semaglutide can cost $1,000, glimepiride might cost $8. For many, especially older adults on fixed incomes, that’s the difference between taking a pill and not taking one at all.
Global sales of sulfonylureas dropped from 26% of the oral diabetes market in 2015 to 18% in 2022. That’s because GLP-1 agonists and SGLT2 inhibitors are taking over. But in low-income countries and among uninsured patients, sulfonylureas still dominate.
Dr. Matthew Riddle warns: “Abandoning sulfonylureas entirely would create access disparities.” They’re not going away. But they should be used more carefully.
What’s Next for Sulfonylureas?
New combinations are coming. Glyburide-metformin XR, for example, is designed to reduce weight gain while keeping blood sugar low. Early results show 1.8 kg less weight gain than glyburide alone.
Researchers are also looking at modified sulfonylureas that stimulate insulin without affecting fat cells. That’s still years away. But the message is clear: the future of diabetes care isn’t just about lowering sugar-it’s about protecting your whole body.
For now, if you’re on a sulfonylurea and you’re gaining weight, don’t just accept it. Talk to your doctor. Ask about gliclazide. Ask about metformin. Ask about lifestyle changes. Your weight matters as much as your A1C.
Do all sulfonylureas cause weight gain?
No. While glimepiride, glyburide, and glipizide are linked to weight gain, gliclazide is an exception. Studies show gliclazide either causes no weight gain or even leads to slight weight loss over time. This makes it a better choice for people concerned about weight.
Can I lose weight while on sulfonylureas?
Yes, but it’s harder. Sulfonylureas make your body hold onto fat. To lose weight, you’ll need to combine diet changes, regular exercise, and possibly adding metformin. Time-restricted eating has shown strong results-limiting food intake to an 8-hour window can cut weight gain by 78%.
Is gliclazide safer than other sulfonylureas?
Yes, in several ways. Gliclazide has a lower risk of weight gain, less hypoglycemia, and possibly better heart protection compared to glimepiride or glyburide. It’s not a miracle drug, but for many patients, it’s the safest sulfonylurea option.
Why do doctors still prescribe sulfonylureas?
Because they’re cheap and effective. A month of glimepiride can cost under $10, while newer drugs like semaglutide cost over $600. For patients without insurance or with limited income, sulfonylureas are often the only affordable option. But guidelines now recommend using them only when newer drugs aren’t accessible.
Should I stop taking my sulfonylurea if I’m gaining weight?
Don’t stop on your own. But do talk to your doctor. If you’ve gained more than 3% of your body weight in six months, it’s time to discuss alternatives. Switching to gliclazide, adding metformin, or moving to a GLP-1 agonist may be better long-term choices.


Kathy Pilkinton
October 30, 2025 AT 07:19Let me guess - your doctor handed you glimepiride like it was a free candy bar and said ‘just take it.’ No discussion, no alternatives, just ‘here’s the cheap one.’ I’ve been there. Gained 18 pounds in a year. My A1C looked fine but my jeans didn’t. Switched to gliclazide. Lost it all. No magic, just less insulin flooding my fat cells. Stop accepting weight gain as ‘normal.’ It’s not. It’s a side effect you can fight.
And yes, I’m mad. Because this isn’t medical care - it’s cost-cutting disguised as treatment.
Holly Dorger
October 31, 2025 AT 11:03i read this whole thing and i just want to say thank you. i was on glyburide for 3 years and thought the weight gain was just me being lazy. turns out it was the drug. switched to gliclazide last year and my energy is back. i still mess up my diet sometimes but at least my body isnt fighting me anymore. also i spell bad sorry. typing on phone while nursing my kid and my coffee.
gliclazide is the quiet hero of diabetes meds. no one talks about it but it works.
Amanda Nicolson
November 1, 2025 AT 08:28Okay, I need to scream into the void about this. I’ve been on sulfonylureas since 2019. I lost 30 pounds on metformin. Then my insurance dropped coverage and suddenly I’m on glipizide. Within six months, I was back to my highest weight ever. I cried in the grocery store because I couldn’t fit into my favorite jeans. I felt like my body was betraying me - but it wasn’t me. It was the damn drug.
And now? I’m on gliclazide. I’ve lost 11 pounds in four months. My doctor didn’t even mention it as an option until I asked. Why? Because no one tells you this stuff. Why are we still letting people get handed these weight-gain bombs like they’re harmless? This isn’t just about numbers on a scale - it’s about dignity, mental health, and survival. I’m not just diabetic. I’m a human being trying not to drown in insulin-induced fat storage.
And if you’re reading this and you’re on glimepiride? Please. Talk to your doctor. Ask for gliclazide. It’s not a miracle. But it’s a lifeline.
Jackson Olsen
November 3, 2025 AT 07:53Penny Clark
November 4, 2025 AT 17:58thank you for writing this. i’ve been on glimepiride for 4 years and thought i was just bad at eating right… turns out my body was just storing everything like a squirrel in winter 😔
i started time-restricted eating (10am-6pm) last month and already lost 3 lbs. i didn’t even change what i ate, just when. it’s like my body finally got a break from insulin spikes. i’m not a diet person but this feels… doable?
also gliclazide sounds like a magic word. i’m asking my dr next week. fingers crossed 🤞
Niki Tiki
November 5, 2025 AT 11:19why are we even talking about this? america is broke so we give people cheap pills. if you can’t afford semaglutide then tough luck. you want to lose weight? stop eating carbs. stop being lazy. this isn’t rocket science. my grandpa took sulfonylureas in the 70s and he lived to 92. stop whining about weight gain. your problem is you eat too much pizza.
and gliclazide? sounds like a brand of yogurt. who cares. just take your damn pill.
Jim Allen
November 6, 2025 AT 15:57so basically insulin = fat storage. big shocker. we’ve known this since the 80s. but now we’re pretending it’s a ‘new discovery’? lol. the system’s broken. Pharma sells us drugs that make us gain weight because then we need more drugs to fix the problems those drugs caused.
it’s not medicine. it’s a business model.
gliclazide? yeah, it’s better. but it’s still insulin-stimulating. we need drugs that don’t force your body to hoard fat. until then, we’re just rearranging deck chairs on the Titanic.
also - 8-hour eating window? sounds like intermittent fasting. yeah, that helps. but it’s not a cure. it’s damage control.
we’re treating symptoms, not causes. and that’s the real tragedy.
Nate Girard
November 6, 2025 AT 20:26I just want to say - if you’re reading this and you’re scared or overwhelmed, you’re not alone. I was on glimepiride for two years and felt like I was failing every day because the scale wouldn’t budge. I thought it was my willpower. It wasn’t. It was the drug.
Switching to gliclazide + metformin + walking 30 minutes a day changed everything. I didn’t ‘fix’ myself - I just stopped fighting my biology. And now I’m not just surviving - I’m actually feeling like myself again.
If you’re hesitant to talk to your doctor, start with this: ‘I’ve gained X pounds on this med. Is there a better option?’ You deserve care that doesn’t punish you for being sick.
Carolyn Kiger
November 7, 2025 AT 18:44My mom is 72 and on glimepiride. She’s on a fixed income. She told me she can’t afford the new drugs. I read this article and cried. She’s not lazy. She’s not undisciplined. She’s just trying to survive in a system that treats affordability as a medical decision.
Thank you for mentioning gliclazide. I’m printing this out and taking it to her next appointment. Maybe we can finally get her off the weight-gain pill. She deserves better than being told ‘it’s just a side effect.’
And to everyone who says ‘just eat less’ - you don’t know what it’s like to be told your medicine is your only option. Please be kind.
krishna raut
November 8, 2025 AT 12:01Gliclazide works. Less weight gain. Less hypoglycemia. Used widely in India. Cost: $2/month. Why not use it more? Simple answer: marketing. Not science.