Top Medication Safety Questions to Ask at the Pharmacy Counter
 Feb, 2 2026
Feb, 2 2026
Every year, hundreds of thousands of people end up in emergency rooms because of mistakes with their medications. Some of these errors happen because someone didn’t know to ask the right questions at the pharmacy. You’re not alone if you’ve ever left the counter feeling unsure about what you were given. That’s why knowing what to ask before you walk away can stop a serious problem before it starts.
What is this medication actually for?
It sounds simple, but many people don’t know why they’re taking a pill. Your doctor might have said it’s for high blood pressure, but the label just says "Lisinopril 10 mg." What does that even mean? Ask your pharmacist: "What is this medication used for?" This isn’t just about understanding your condition-it’s about catching mistakes. I’ve seen cases where someone was given a thyroid med by accident because the label looked similar to their real prescription. If you know what the medicine is supposed to do, you’ll notice if it’s not working-or if it’s doing something it shouldn’t.
How and when should I take this?
"Take one daily" doesn’t cut it. When? Morning? Night? With food? On an empty stomach? Some meds need to be taken at the same time every day to stay effective. Others can cause stomach upset if taken without food. A blood pressure pill might need to be taken in the morning so it doesn’t mess with your sleep. A diabetes drug might need to be timed with meals. And don’t assume "once daily" means anytime. Some meds lose their effect if taken at the wrong time. Ask for specifics: "Should I take this before breakfast, after dinner, or at bedtime?" If the bottle says "take with food," ask what kind of food works best. A small snack? A full meal? This detail matters.
What side effects should I watch for?
Everyone hears about common side effects like dizziness or nausea. But what’s dangerous? What’s normal? Ask: "Which side effects mean I need to call my doctor right away?" Some meds can cause internal bleeding, liver damage, or dangerous drops in blood pressure-all of which might start with subtle signs. For example, if you’re on a blood thinner like warfarin, a slight bruise might seem harmless. But if you start bleeding from your gums, passing dark stools, or getting headaches with vision changes, that’s an emergency. Your pharmacist knows which symptoms are red flags. They’ve seen the worst-case scenarios. Don’t wait until you’re panicked to find out what’s serious.
Does this interact with anything else I’m taking?
This is the one question most people forget to ask. It’s not just about other prescription drugs. It’s about your daily vitamins, herbal supplements, even over-the-counter painkillers. I’ve had patients come in with a list of 12 different pills-some bought online, some given to them by a friend. One man was taking turmeric for joint pain and didn’t realize it was making his blood thinner way too strong. He ended up in the hospital with internal bleeding. Ibuprofen and warfarin? That combo increases bleeding risk by 40-60%. St. John’s Wort can make antidepressants useless or cause serotonin syndrome. Even grapefruit juice can turn a common cholesterol pill into a dangerous overdose. Bring everything-pills, gummies, teas, patches-to the pharmacy. Let them see it all.
Is there anything in this that could trigger an allergy?
You might know you’re allergic to penicillin. But what about dyes, fillers, or preservatives? Some pills have red dye that can cause hives. Others contain lactose, gluten, or soy-ingredients you might not expect. If you’ve ever broken out in a rash after starting a new med, that’s not just bad luck. Ask: "Does this contain any ingredients I should avoid because of allergies?" Pharmacists check the inactive ingredients, not just the active ones. They’ve seen people react to colors, coatings, or even the shape of the pill. If you’ve had a reaction before, tell them exactly what happened. That info saves lives.
How do I store this properly?
Most people keep their meds in the bathroom cabinet. Bad idea. Heat and moisture ruin pills. Insulin? It goes bad if left in a hot car. Antibiotics? Some need refrigeration. Eye drops? Once opened, they expire in 28 days-even if the bottle says "use by 2027." Ask: "Where should I keep this?" And don’t assume the original bottle is fine. If you transfer pills to a pill organizer, make sure you know what each one is. I’ve seen people mix up blood pressure meds and thyroid pills in the same container. One wrong pill can cause a stroke. Keep meds in their original containers. If you need a pill box, label each compartment clearly.
Can I repeat this back to you to make sure I got it right?
This is the secret weapon most people don’t use. Ask: "Can I repeat what you just told me so you can check if I understood?" It sounds awkward, but pharmacists love it. A 2020 study found that patients who did this reduced communication errors by 31%. You say: "So this is for my cholesterol, I take one in the evening with food, and if I get muscle pain or dark urine, I need to call you right away?" The pharmacist will correct you if you missed something. It’s not about doubting them-it’s about making sure you’re both on the same page. This simple step has prevented countless mistakes in clinics and hospitals.
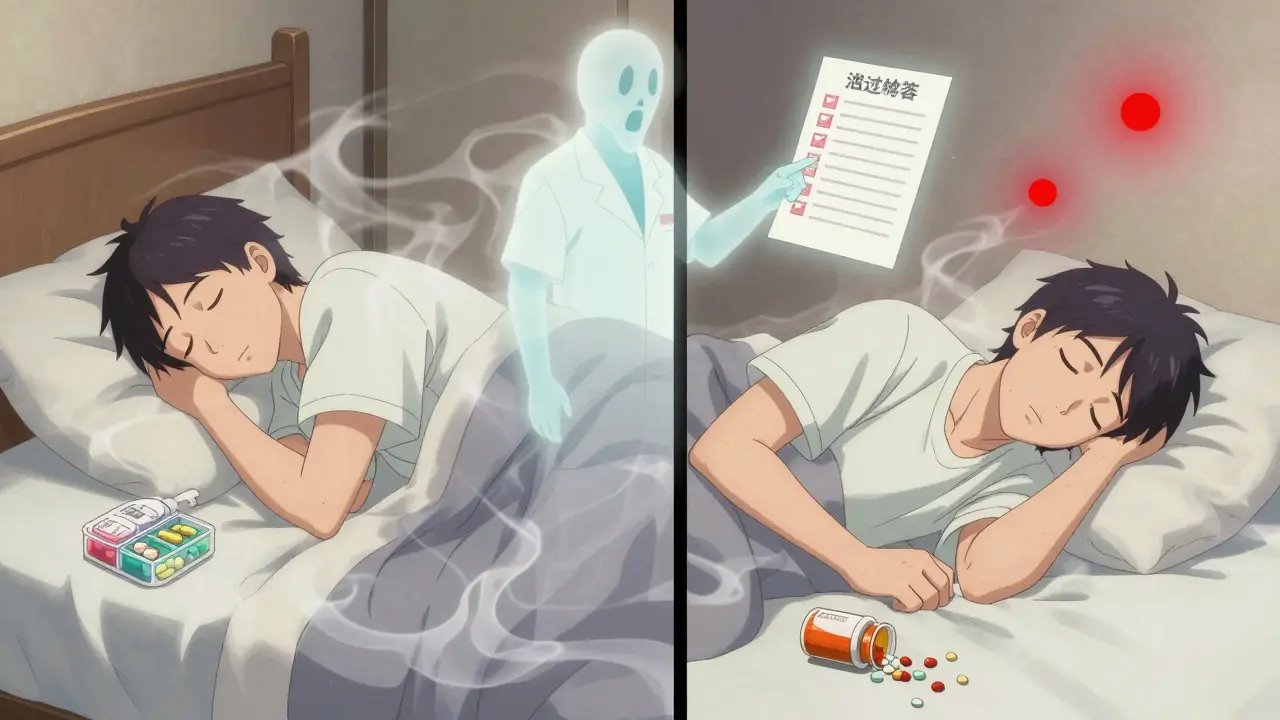
What if I miss a dose?
Life happens. You oversleep. You’re traveling. You forget. What do you do? Don’t guess. Don’t double up unless you’re told to. Some meds are safe to take late. Others can cause dangerous spikes in blood pressure or heart rate. For example, missing a dose of a beta-blocker might cause your heart to race. Missing a dose of an antibiotic could let bacteria grow back stronger. Ask: "If I forget to take this, what should I do?" Write down the answer. Keep it on your phone. That way, you’re not scrambling when it happens.
Do I need to avoid any foods, drinks, or activities?
Some meds make you sensitive to sunlight. You might get a bad sunburn just walking to your car. Others can make you dizzy, so driving isn’t safe. Some raise your blood pressure if you drink coffee. A few interact with alcohol in ways that can cause liver damage. Ask: "Is there anything I should avoid while taking this?" Even something as simple as eating grapefruit can turn a common statin into a toxic dose. Your pharmacist knows which foods, drinks, or activities could turn a safe med into a risk.
What should I do if I don’t feel right?
Too many people wait until they’re in crisis before calling anyone. If you feel off-headaches, nausea, unusual fatigue, mood changes-don’t assume it’s just stress. Ask your pharmacist: "What should I do if I start feeling worse after starting this?" They’ll tell you which symptoms are normal and which need immediate attention. Keep their number handy. Many pharmacies offer free 24/7 medication advice lines. Use them. You don’t need to wait for your doctor’s office to open.
Why does this look different than last time?
Ever open a new bottle and think, "This pill doesn’t look right?" It might be the same medicine, just from a different manufacturer. But it might not be. Ask: "Is this the same medication I got last time?" The color, shape, or imprint might change, but the name and dose should be the same. If it looks completely different, double-check. The Institute for Safe Medication Practices says 18% of dispensing errors involve the wrong pill being handed out because the patient didn’t question the appearance. Don’t be shy. Hold it up. Ask. Better safe than sorry.
Should I keep taking this long-term?
Some meds are meant to be taken for life. Others are short-term. But many people keep taking things they were given years ago-painkillers, sleep aids, even antibiotics. Ask: "Do I still need this? Should I be on it long-term?" Your pharmacist can help you review your whole list. They’ll spot duplicates, outdated prescriptions, or meds that might be doing more harm than good. A 2022 Johns Hopkins study showed that bringing all your meds to a pharmacy review reduced dangerous polypharmacy by nearly 30%.
How do I safely stop taking this?
You can’t just quit some meds cold turkey. Blood pressure pills, antidepressants, steroids-stopping suddenly can cause rebound effects, seizures, or even heart attacks. Ask: "How do I stop this safely?" If you want to stop, your pharmacist can help you taper off slowly. They’ll tell you how long to wait between doses and what symptoms to watch for. Never assume it’s safe to stop on your own.
What if I’m traveling?
Time zones, lost luggage, different climates-all of this affects your meds. Ask: "What should I do if I’m traveling?" Keep meds in your carry-on. Bring extra in case of delays. Check if your meds are allowed in the country you’re visiting. Some countries ban common painkillers or ADHD meds. Ask about storage if you’re going somewhere hot. And always carry a list of your meds and dosages-paper copy, not just on your phone.
Can you help me organize my meds?
If you’re taking five or more pills a day, it’s easy to get confused. Ask if your pharmacy offers blister packs, dosette boxes, or automated dispensers. Many pharmacies now give you a weekly organizer with your meds already sorted by time of day. It’s free or low-cost. It reduces errors. It saves time. And it’s especially helpful for older adults or anyone managing chronic conditions.
What if I have more questions later?
Don’t wait until you’re in panic mode. Ask: "How can I reach you if I have more questions after I leave?" Most pharmacies have a phone line, email, or even a chat feature on their website. Write down the contact info. Save it in your phone. This isn’t a one-time conversation. Medication safety is ongoing. You’re not bothering them. You’re doing your part to stay safe.
What’s the most important question to ask at the pharmacy?
The most important question is: "What is this medication for?" If you don’t know why you’re taking it, you can’t tell if it’s working-or if you’ve been given the wrong thing. This simple question catches the most common dispensing errors and helps you understand your treatment plan.
Can I ask questions even if I’ve taken the medication before?
Yes, absolutely. Medications can change-dosage, manufacturer, or even ingredients. Your body changes too. What was safe last year might not be safe now, especially if you’ve started a new drug, supplement, or health condition. Always confirm, even with familiar meds.
Do pharmacists really catch dangerous interactions?
Yes. A 2022 survey by the American Pharmacists Association found that 89% of pharmacists identify potentially harmful drug interactions during patient consultations. They prevent serious adverse events in 67% of those cases just by speaking up.
Is it okay to bring all my medications to the pharmacy?
Yes, and you should. Bring every pill, vitamin, supplement, cream, eye drop, and patch-even the ones you haven’t used in months. This lets the pharmacist see your full picture. A 2022 Johns Hopkins study showed this reduces dangerous drug combinations by 29%.
What if I’m embarrassed to ask questions?
You’re not being annoying-you’re being smart. Pharmacists are trained to answer questions. They’ve seen hundreds of patients. The ones who ask questions are the ones who stay safe. If you feel rushed, ask to speak with the pharmacist privately. Most pharmacies have quiet consultation rooms. Your safety is their job.

