Transient Ischemic Attack & Diabetes: How They’re Connected
 Oct, 14 2025
Oct, 14 2025
TIA Risk Assessment Calculator
TIA Risk Assessment
This tool estimates your risk of Transient Ischemic Attack based on key diabetes management factors. Remember: TIAs are medical emergencies requiring immediate attention.
When a brief, brain‑fogging episode pops up, most people think it’s just a migraine or fatigue. In reality, a Transient Ischemic Attack (TIA) is a warning sign that the blood‑flow pathways to the brain are under stress, and if you’re living with diabetes, that stress can be far higher. This article breaks down what a TIA is, why diabetes makes it more likely, and what you can do right now to lower the odds of a serious stroke.
Key Takeaways
- A TIA is a short‑lasting neurological event that signals a temporary loss of blood flow to the brain.
- People with Diabetes Mellitus face a 30‑50% higher risk of a TIA compared with non‑diabetics.
- High blood glucose, accelerated atherosclerosis, and co‑existing hypertension are the main culprits.
- Recognizing TIA symptoms and seeking immediate care can prevent a full‑blown stroke.
- Strict glycemic control, blood‑pressure management, and healthy lifestyle choices cut TIA risk dramatically.
What Is a Transient Ischemic Attack?
Transient Ischemic Attack is a brief neurological episode caused by a temporary blockage of blood flow to part of the brain. The blockage usually clears within minutes, so symptoms resolve within 24 hours-often in just a few minutes. Because the brain tissue survives, there’s no permanent damage, but the event serves as a stark alarm that the vascular system is on the brink of a larger insult, typically a stroke.
Typical manifestations include sudden weakness or numbness on one side of the body, difficulty speaking, vision loss in one eye, or a loss of balance. The acronym “FAST” (Face drooping, Arm weakness, Speech difficulty, Time to call emergency services) works just as well for TIAs as it does for strokes.
Diabetes Mellitus: A Quick Overview
Diabetes Mellitus is a chronic metabolic disorder characterized by elevated blood‑glucose levels due to insufficient insulin production, insulin resistance, or both. Roughly 1 in 10 adults worldwide live with either type1 or type2 diabetes, and the condition brings a host of vascular complications that affect both small vessels (microvascular) and large vessels (macrovascular). The macrovascular side-particularly atherosclerosis-directly links diabetes to brain‑related events like TIA and stroke.
How Diabetes Raises TIA Risk
The relationship between diabetes and TIA isn’t a single‑factor story. Several interlocking mechanisms create a perfect storm:
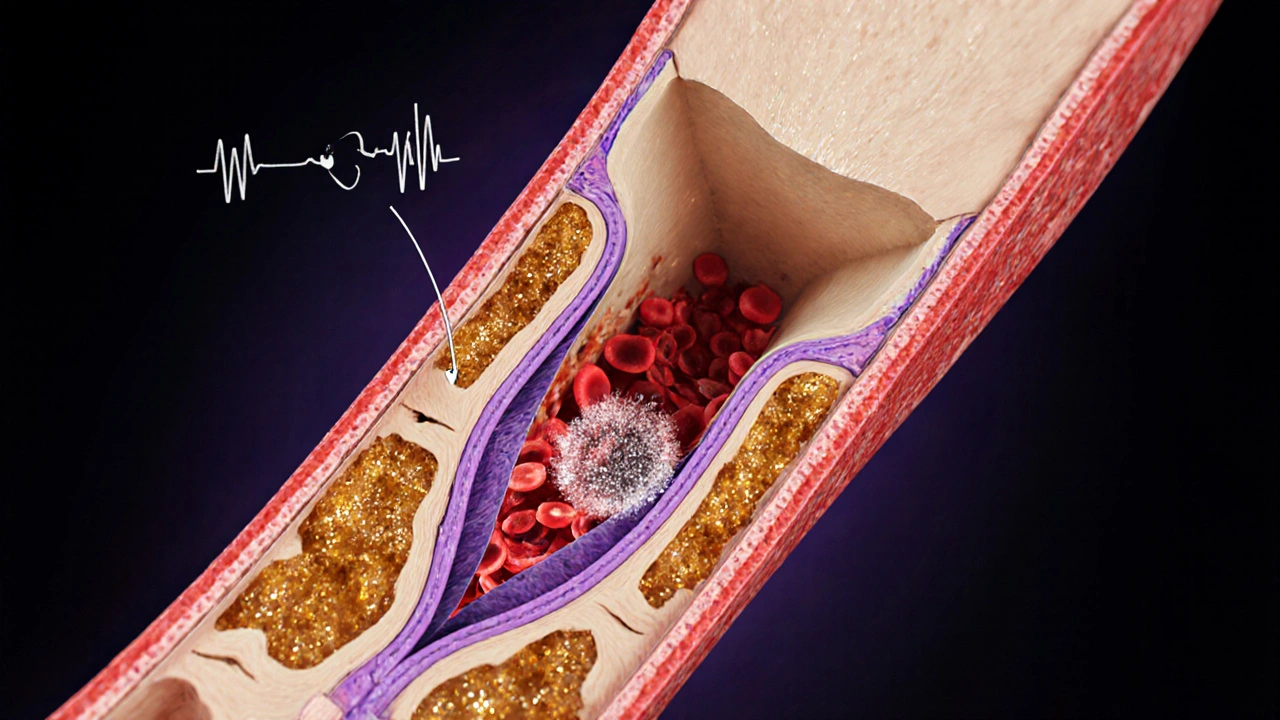
- Accelerated atherosclerosis: High glucose levels damage the inner lining of arteries, prompting plaque buildup. The carotid arteries, which supply the brain, become narrowed, making them prone to temporary clots.
- Hyperglycemia‑induced inflammation: Excess glucose spurs inflammatory pathways, increasing the likelihood that a small clot forms and briefly blocks cerebral vessels.
- Elevated HbA1c: The hemoglobin A1c test reflects average blood sugar over the past three months. Studies published in 2023 show that patients with HbA1c>8% have a 1.8‑fold higher odds of a TIA than those with HbA1c<6.5%.
- Co‑existing hypertension: Diabetes often co‑exists with high blood pressure. The combination multiplies the risk; a meta‑analysis of 15 studies found a synergistic risk increase of 2.5 times for TIA when both conditions are present.
- Altered platelet function: High glucose makes platelets stickier, encouraging tiny clots that can travel to the brain and cause a brief blockage.
Because these mechanisms act together, the overall relative risk for a TIA in diabetics hovers around 1.3 to 1.5 compared with non‑diabetics, depending on age and control level.
Spotting a TIA: Symptoms to Watch
Time matters. If you think you or someone else is having a TIA, call emergency services right away. Common signs include:
- Sudden weakness or numbness in the face, arm, or leg-usually on one side.
- Difficulty speaking or slurred words.
- Blurred or double vision, or loss of vision in one eye.
- Dizziness, loss of balance, or trouble walking.
- Sudden, severe headache with no known cause.
Even if symptoms disappear within minutes, they shouldn’t be ignored. A brief episode is often the first cue that a larger stroke could follow.
What Happens After a TIA? Diagnosis and Immediate Steps
Medical professionals typically run a series of tests to pinpoint the cause and assess future risk:
- Neuroimaging: A non‑contrast CT scan rules out bleeding; an MRI with diffusion‑weighted imaging catches subtle brain changes.
- Carotid ultrasound: Measures plaque buildup in the carotid arteries. If narrowing exceeds 70%, surgery or stenting may be recommended.
- Blood work: Includes fasting glucose, HbA1c, lipid panel, and coagulation studies.
- Electrocardiogram (ECG) and cardiac monitoring: Detect atrial fibrillation, a common source of embolic TIAs.
Based on these results, doctors craft a personalized plan that often includes medication, lifestyle tweaks, and close follow‑up.
Prevention Strategies for People with Diabetes
Reducing TIA risk boils down to three pillars: control blood sugar, protect the vessels, and adopt a heart‑healthy lifestyle.
- Maintain target HbA1c: Aim for 7% or lower (or as advised by your endocrinologist). Consistent monitoring-through home glucometers and quarterly lab tests-keeps you on track.
- Manage blood pressure: Keep systolic pressure below 130mmHg. ACE inhibitors or ARBs are often first‑line for diabetics because they also protect kidney function.
- Control cholesterol: Statins reduce LDL cholesterol and have been shown to lower stroke risk by up to 20% in diabetics.
- Consider antiplatelet therapy: Low‑dose aspirin (81mg) or clopidogrel may be prescribed after a TIA, especially if you have other risk factors. Antiplatelet therapy works by preventing platelets from clumping together, reducing clot formation.
- Adopt a Mediterranean‑style diet: Emphasize whole grains, oily fish, nuts, olive oil, and plenty of vegetables. This pattern improves insulin sensitivity and reduces inflammation.
- Stay active: At least 150 minutes of moderate aerobic exercise per week-walking, cycling, swimming-helps lower glucose, blood pressure, and weight.
- Quit smoking: Tobacco accelerates atherosclerosis and makes platelets stickier.
- Regular screening: Annual retinal exams, foot checks, and especially carotid ultrasounds for those over 55 or with a previous TIA.

Managing a TIA When It Occurs
If a TIA does happen, the goal shifts to preventing a full stroke. Treatment generally follows these steps:
- Hospital admission: Most patients are observed for 24‑48hours to monitor for a subsequent stroke.
- Start or adjust antiplatelet meds: If you’re not already on aspirin, it’s usually started within 24hours.
- Address underlying causes: This might involve carotid endarterectomy, intensive blood‑pressure control, or anticoagulation if atrial fibrillation is discovered.
- Intensive diabetes management: In‑hospital glucose targets often sit between 140‑180mg/dL; post‑discharge, the focus returns to personalized HbA1c goals.
- Rehabilitation and education: Physical therapy, speech therapy, and a clear plan for medication adherence are essential for recovery and future risk reduction.
Follow‑up appointments usually occur within two weeks, then at three‑month intervals for the first year.
Risk Comparison: Diabetics vs. Non‑Diabetics
| Group | Annual TIA Incidence (per 100,000) | Relative Risk (RR) |
|---|---|---|
| Non‑Diabetic adults (40‑70 y) | 45 | 1.0 (baseline) |
| Diabetics, well‑controlled (HbA1c <7%) | 68 | 1.5 |
| Diabetics, poorly controlled (HbA1c ≥8%) | 94 | 2.1 |
| Diabetics with additional hypertension | 112 | 2.5 |
These numbers come from a 2024 population‑based cohort in Australia and Europe, underscoring how tighter glucose control can shave off dozens of TIA events per 100,000 people each year.
Frequently Asked Questions
Can a TIA be completely prevented?
While no one can guarantee 100% prevention, managing diabetes, blood pressure, cholesterol, and lifestyle factors can reduce the risk by 40‑60% according to recent clinical guidelines.
Is a TIA the same as a mini‑stroke?
Yes, a TIA is often called a “mini‑stroke” because it involves the same blood‑flow interruption but the symptoms resolve within 24 hours and typically leave no permanent damage.
Should I take aspirin daily if I have diabetes?
Aspirin is not automatically prescribed to every diabetic. Your doctor will weigh your personal stroke risk, bleeding risk, and any other medications before recommending a low‑dose regimen.
How quickly do I need to see a doctor after a TIA?
Treat it as an emergency. Call emergency services immediately; the sooner you get evaluated, the better the chance of preventing a full stroke.
Does type1 diabetes carry the same TIA risk as type2?
Both types increase risk, but type2 is more often accompanied by hypertension, dyslipidemia, and obesity, which amplify the TIA probability. Nevertheless, uncontrolled type1 also raises risk due to chronic hyperglycemia.
Next Steps for Readers
If you have diabetes, start by reviewing your most recent HbA1c and blood‑pressure numbers. Schedule a check‑up with your primary care doctor to discuss whether a carotid ultrasound is appropriate for you. Consider setting up a recurring reminder to log daily glucose readings and keep a symptom diary-any fleeting weakness or vision change should prompt an urgent call to your health provider.
Remember, a brief episode is a courtesy call from your body. Respond quickly, manage your diabetes proactively, and you can dramatically lower the chance that a TIA turns into a disabling stroke.


Boston Farm to School
October 15, 2025 AT 05:46Interesting read on TIA risks for diabetics :)
Emily Collier
October 15, 2025 AT 07:10The link between hyperglycemia and vascular inflammation is clearly explained here. It’s reassuring to see actionable steps outlined for blood‑pressure control and HbA1c management. Maintaining a target HbA1c below 7 % can significantly lower the risk of a transient ischemic attack. Regular check‑ups with a primary care provider or endocrinologist will keep these numbers in check. Keep up the good work on sharing valuable health information.
Catherine Zeigler
October 15, 2025 AT 08:33Living with diabetes adds a layer of complexity to vascular health that many people underestimate. First, chronic hyperglycemia accelerates endothelial dysfunction, which compromises the integrity of the blood‑brain barrier. Second, the resulting oxidative stress promotes plaque formation in the carotid arteries, making them prone to rupture or transient blockage. Third, elevated HbA1c levels have been associated with a roughly two‑fold increase in TIA incidence across multiple cohort studies. Moreover, hypertension frequently co‑exists with diabetes, creating a synergistic effect that magnifies stroke risk. Lifestyle factors such as smoking further tip the balance toward vascular events. That is why regular monitoring of blood pressure, glucose, and cholesterol is essential. Patients should aim for an HbA1c below 7 % while also keeping systolic pressure under 130 mmHg when possible. In addition to medication adherence, incorporating aerobic exercise at least three times a week can improve endothelial function. A balanced diet rich in whole grains, lean proteins, and healthy fats supports both glycemic control and vascular health. Stress management techniques, including mindfulness meditation, have shown modest benefits in reducing inflammatory markers. Importantly, any new neurological symptom-however brief-warrants immediate medical evaluation. Time is brain; the faster a TIA is addressed, the lower the chance of a full‑blown stroke. Clinicians often recommend antiplatelet therapy after a TIA, especially when risk factors cluster. Finally, patient education empowers individuals to recognize warning signs and seek care without delay. Staying proactive with regular check‑ups can keep you one step ahead of potential complications.
henry leathem
October 15, 2025 AT 09:56The pathophysiology described borders on the speculative, lacking mechanistic rigor. Additionally, the author overstates the causal link without sufficient citation.
jeff lamore
October 15, 2025 AT 11:20Thank you for compiling these data points. They serve as a concise reminder of the importance of tight glycemic control.
Kris cree9
October 15, 2025 AT 12:43Wow, this is like a wake‑up call from the universe lol. I totally felt the drama of a TIA looming!
John Babko
October 15, 2025 AT 14:06We must prioritize American healthcare reforms!!! Our patients deserve the best interventions-no more delays!!!
Stacy McAlpine
October 15, 2025 AT 15:30I hear you, but let’s keep the conversation focused on evidence‑based strategies rather than politics.
Roger Perez
October 15, 2025 AT 16:53Exactly! 😊 The data shows lifestyle changes can cut risk by half, so let’s spread the word!
Ian McKay
October 15, 2025 AT 18:16The article correctly cites recent studies; however, it omits a discussion of antiplatelet therapy, which is a key component of post‑TIA management.
Kristen Holcomb
October 15, 2025 AT 19:40Everyone reading should know that managing stress is just as crucial as meds-don’t forget mindfulness!
justin davis
October 15, 2025 AT 21:03Great, another checklist-because we all love more paperwork!!!
David Lance Saxon Jr.
October 15, 2025 AT 22:26One might argue that the epistemic framework underlying TIA risk assessment is fundamentally flawed, yet practical application persists.
Stu Davies
October 15, 2025 AT 23:50Sending supportive thoughts to anyone who’s experienced a TIA 😔.
Benjamin Cook
October 16, 2025 AT 01:13Thanks for the info-really helpful! Hope you all stay healthy!