Warfarin and Vitamin K Foods: How to Keep Your Diet Consistent for Safe Blood Thinning
 Dec, 8 2025
Dec, 8 2025
When you’re on warfarin, your diet isn’t about eating healthy or avoiding certain foods-it’s about keeping it the same. It’s not the vitamin K in your spinach that’s dangerous. It’s the sudden change in how much you eat from day to day. One week you’re eating a salad with a cup of cooked kale, the next you’re skipping greens for pasta. That’s when your INR starts to swing, and your risk of clotting or bleeding goes up.
Why Vitamin K Matters With Warfarin
Warfarin works by blocking vitamin K’s role in making blood clot. Without enough active vitamin K, your body can’t produce clotting factors like II, VII, IX, and X. That’s why your blood thins. But here’s the catch: your body needs vitamin K for other things too-bone health, artery protection, even cell function. So you can’t just cut it out. You have to keep it steady.The key number doctors watch is your INR. That’s the International Normalized Ratio. A reading between 2.0 and 3.0 is the sweet spot for most people on warfarin. If your INR drops below 2.0, your blood clots too easily. Above 3.0, you’re at higher risk of bleeding. And vitamin K intake? It can shift your INR by 0.5 to 1.0 points with just a 100-microgram change in daily intake. That’s the equivalent of one extra cup of cooked spinach.
Studies show that people with unstable INR aren’t necessarily eating more vitamin K-they’re eating inconsistent amounts. One study found that those whose daily vitamin K intake varied by more than 50% were over three times more likely to have INR levels outside the safe range. That’s not about being bad at dieting. It’s about how unpredictable your intake is.
What Foods Are High in Vitamin K?
Vitamin K1, the kind that affects warfarin, comes mostly from plants. Here’s what’s packed with it:- Cooked kale: 1,062 mcg per cup
- Cooked spinach: 889 mcg per cup
- Cooked Brussels sprouts: 156 mcg per cup
- Raw Swiss chard: 299 mcg per cup
- Raw broccoli: 85 mcg per cup
- Asparagus: 70 mcg per cup
- Green tea: 41-88 mcg per serving
These aren’t obscure superfoods-they’re common vegetables. You don’t need to avoid them. You just need to know how much you’re eating and stick to it.
Don’t forget: vitamin K2, found in fermented foods like natto, cheese, and egg yolks, also plays a role. But it makes up less than 10% of most people’s intake. So for most warfarin users, the real issue is leafy greens.
Consistency Over Restriction
You’ve probably heard conflicting advice: “Avoid greens,” “Eat more greens,” “Just don’t touch them.” Here’s the truth: Don’t avoid vitamin K-rich foods. Just keep your intake steady.The American Heart Association, the Anticoagulation Forum, and the Mayo Clinic all agree: consistency beats restriction. Eating two cups of cooked spinach every Tuesday and Thursday? That’s fine. Eating a big salad on Monday, then nothing for four days? That’s the problem.
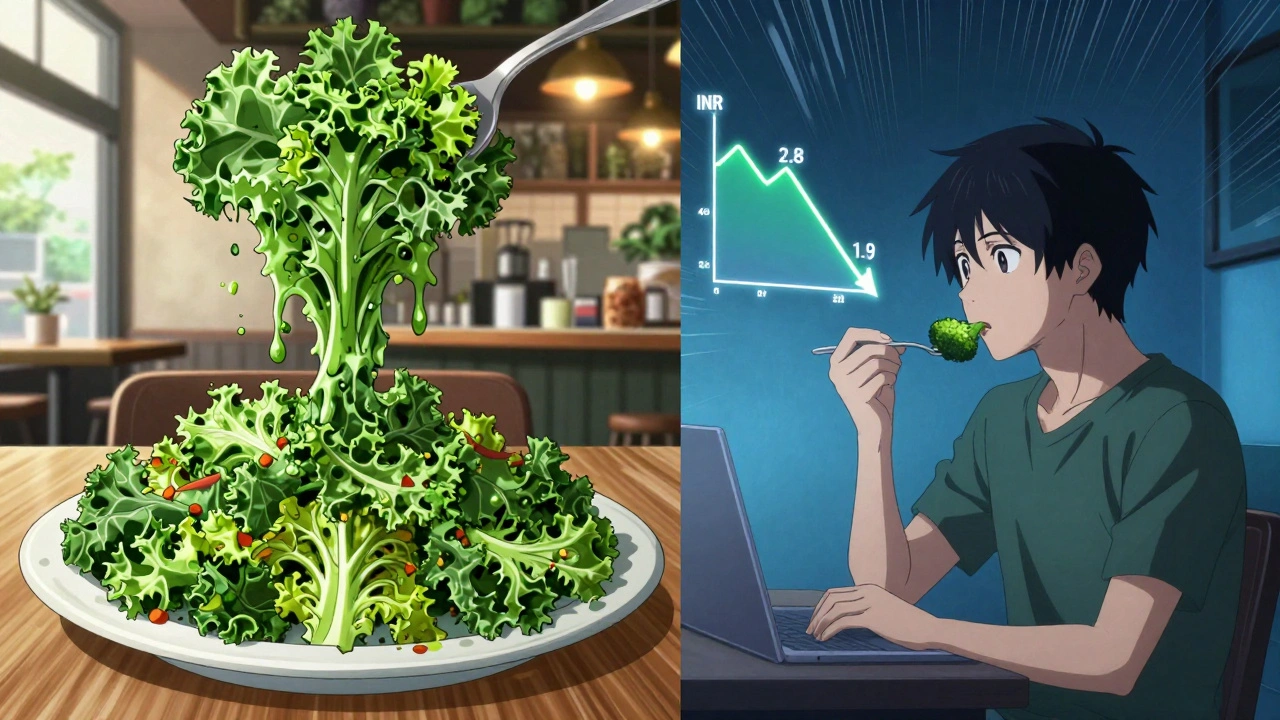
One patient tracked his intake for six months. He ate exactly two cups of cooked spinach twice a week. His INR stayed rock solid for eight years. Another patient, after a “cleanse” that included three days of kale salads, saw his INR crash from 2.8 to 1.9. He needed a 15% dose increase. That’s not a coincidence. That’s how sensitive warfarin is.
Research from the University of North Carolina shows that patients who got personalized diet counseling from a registered dietitian hit their target INR 85% of the time. Those who didn’t? Only 65%. That’s a huge gap. And it’s not because the dietitians gave them a magic list. They taught them how to be consistent.
How to Track Your Vitamin K Intake
You don’t need to count micrograms every day. But you do need to notice patterns.- Use measuring cups for leafy greens. A handful isn’t a cup. A cup of raw spinach cooks down to about 1/4 cup. That’s a big difference.
- Keep a simple food diary. Note the days you eat kale, spinach, broccoli, or green tea. Don’t overcomplicate it. Just write it down.
- Be aware of restaurant meals. A “healthy” salad at a café might have two cups of spinach and kale. That’s more than double what you usually eat.
- If you take a multivitamin, make sure it’s the same brand and dose every day. Some contain vitamin K. Others don’t. Switching brands can throw off your INR.
- Seasonal changes matter. If you eat more greens in summer, plan for it. Eat the same amount in winter-even if it’s frozen or canned.
One man in Sydney stopped eating raw kale in winter because it was expensive and hard to find. He switched to frozen spinach, kept the portion the same, and his INR never budged. He didn’t change his diet-he changed how he accessed it.
What to Do After a Big Vitamin K Meal
Life happens. You go out to dinner. You get a free kale salad at a promotion. You eat three servings of broccoli because you’re hungry.If you eat more than double your usual vitamin K intake in one day, your INR will likely drop in the next few days. You won’t feel it. But your blood will clot faster.
Here’s what to do:
- Don’t change your warfarin dose on your own.
- Call your anticoagulation clinic or doctor. Tell them what you ate.
- They might ask you to come in for an INR test sooner than scheduled.
- If your INR drops below 2.0, they may increase your warfarin dose by 10-20% for a few days.
Some clinics even use tools that factor in your vitamin K intake when calculating your dose. A 2020 study showed this improved time in range by over 12%. That’s not science fiction. That’s real, current practice.
What Not to Do
There are three big mistakes people make:- Going on a green juice cleanse. One cup of kale juice can contain over 2,000 mcg of vitamin K. That’s more than double your weekly intake. Your INR will crash.
- Switching to a vegan or Mediterranean diet without planning. These diets are great-but if you suddenly add tons of greens, your INR will drop. Talk to your doctor before making big changes.
- Assuming all greens are equal. Raw spinach has less vitamin K than cooked. Boiling reduces vitamin K by about 30%. Steaming preserves it. Know how your food is prepared.
And never stop taking warfarin because you’re worried about your diet. That’s more dangerous than any vegetable.

When to Get Help
You don’t need to figure this out alone. Reach out if:- Your INR has been out of range twice in three months.
- You’ve changed your diet, started a new supplement, or gotten sick.
- You’re eating more or less greens than usual and don’t know how to adjust.
Most anticoagulation clinics offer free diet counseling. A registered dietitian who knows warfarin can help you build a simple, repeatable plan. You don’t need to memorize numbers. You just need to be predictable.
Real Talk: It’s Not Perfect
I’ve talked to people who’ve been on warfarin for 15 years. Some say it’s the hardest part of their life. Others say it’s just part of their routine.One woman in Adelaide eats one cup of cooked spinach every Monday and Thursday. She never eats it on other days. She’s had the same INR for six years. Another man eats a small salad every day with a tablespoon of olive oil and a few leaves of arugula. He doesn’t measure it. He just eats the same thing every day. His INR is stable.
You don’t need to be perfect. You just need to be consistent. Your body doesn’t care if you eat spinach or broccoli. It cares if you eat the same amount, every day.
Can I eat kale if I’m on warfarin?
Yes, you can eat kale-but only if you eat about the same amount every day. A cup of cooked kale has over 1,000 mcg of vitamin K. If you normally eat none, suddenly eating a cup daily will lower your INR. If you already eat a cup every Tuesday and Thursday, keep doing that. Consistency is what keeps your blood thinning stable.
What happens if I eat too much vitamin K?
Eating a lot of vitamin K doesn’t harm your body-it just makes warfarin less effective. Your INR will drop, meaning your blood clots faster. That raises your risk of stroke, heart attack, or deep vein thrombosis. It’s not an emergency, but it needs to be caught early. Call your doctor if you’ve had a big vitamin K meal and your next INR test is more than a week away.
Should I avoid green tea on warfarin?
Green tea contains vitamin K (41-88 mcg per serving), but it’s not usually a problem unless you drink a lot. One cup a day is fine if it’s consistent. But if you start drinking five cups daily, your INR may drop. The same goes for herbal teas-some, like nettle or alfalfa, are high in vitamin K. Check labels or ask your pharmacist.
Can I take vitamin K supplements?
Only if your doctor says so. Most multivitamins contain vitamin K, and that’s usually fine if you take the same one every day. But taking extra vitamin K supplements without medical advice can interfere with warfarin. If you’re considering supplements, talk to your anticoagulation clinic first.
How often should I get my INR checked?
When you’re stable, every 4 weeks is typical. But if you’ve changed your diet, started a new medication, or gotten sick, your doctor may want you tested sooner-sometimes within 3-7 days. Don’t wait for your next scheduled test if you’ve made a big change. Call ahead.
Is it better to eat low vitamin K or high vitamin K?
Neither. Research shows that people who eat a moderate, consistent amount of vitamin K (75-100 mcg/day) have the most stable INR. Very low intake (under 50 mcg/day) can make warfarin dosing harder to predict. Your goal isn’t to eat less-it’s to eat the same amount every day.
Next Steps
Start today. Pick one thing to keep consistent:- Choose one vitamin K-rich food you eat regularly and measure it with a cup.
- Write down the days you eat it.
- Stick to it for two weeks.
That’s it. No drastic changes. No fear. Just predictability. Your body, and your INR, will thank you.


Courtney Black
December 10, 2025 AT 09:20It’s not about avoiding kale. It’s about treating your diet like a metronome. One beat. Every day. Your body doesn’t care if it’s spinach or swiss chard-it cares if the rhythm stays the same. Change the tempo, and your INR goes haywire. No magic. No miracle foods. Just consistency. That’s the real therapy.
People think they’re being ‘healthy’ by switching up greens. Nah. They’re playing Russian roulette with their blood.
I’ve seen it. A guy ate a big salad on Friday, skipped it all weekend, then had a stroke on Monday. Not because he ate too much. Because he ate too *unpredictably*.
iswarya bala
December 10, 2025 AT 12:14omg this is so relatable!! i was eating so much spinach last month and my dr was like ‘baby u r on warfarin not a rabbit’ 😅 now i eat 1 cup every tuesday n thurs like clockwork. no more ‘healthy cleanse’ nonsense. my inr is stable and i finally sleep at night. thank u for this!!
Simran Chettiar
December 11, 2025 AT 16:38One must consider the philosophical underpinnings of dietary adherence in chronic anticoagulation therapy. The body, as a system of equilibrium, responds not to the absolute quantity of vitamin K, but to the constancy of its flux. To fluctuate is to invite chaos; to stabilize is to embrace harmony. The human organism, though complex, is not designed for caprice. It seeks rhythm. It demands predictability. The modern diet, saturated with inconsistency, is the true adversary-not vitamin K, not warfarin, but the very notion that variety is inherently virtuous.
It is not a diet we must control. It is a ritual we must cultivate. A sacred repetition. A daily affirmation of order against the entropy of convenience.
And yet, we still reach for kale salads on impulse. We still confuse discipline with deprivation. We must learn to eat not to heal, but to remain.
Philippa Barraclough
December 13, 2025 AT 02:17Interesting how the data consistently shows that variability in intake is the primary driver of INR instability-not absolute levels. That’s a subtle but critical distinction. Most patients assume they need to restrict, when the real issue is irregularity. The fact that even a 50% daily fluctuation triples the risk of out-of-range INR is staggering. It suggests that behavioral consistency may be more impactful than pharmacological precision.
Also worth noting: the UNC study’s 85% target INR rate with dietitian support highlights how underutilized nutritional counseling is in anticoagulation clinics. It’s not that the science is lacking-it’s that the system isn’t structured to deliver it. Why isn’t dietitian follow-up standard? Why is it treated as an optional add-on?
And the point about frozen vs. fresh? That’s gold. Seasonal access doesn’t have to mean seasonal inconsistency. It’s about adaptation, not abandonment.
Olivia Portier
December 14, 2025 AT 16:06YOU GOT THIS. Seriously. I know it feels overwhelming at first-like you have to memorize a whole new language. But it’s not about perfection. It’s about showing up the same way, day after day. One cup of spinach on Tues/Thurs? Do it. Same brand of multivitamin? Stick with it. Even if you mess up once? Just reset. No guilt. No shame. You’re not failing-you’re learning.
My friend’s mom did this for 12 years. She ate the same frozen broccoli every night. Same amount. Same time. No drama. Her INR was stable. She traveled, got sick, had holidays-and still kept it simple. You don’t need to be a nutritionist. You just need to be reliable.
Start small. Pick one thing. Do it for two weeks. Then celebrate. You’re doing better than you think.
And if you need someone to cheer you on? I’m here. Always.
Brianna Black
December 15, 2025 AT 11:07Let me be perfectly clear: this is not a diet. This is a covenant. A pact between your body and your survival.
Warfarin does not negotiate. It does not forgive inconsistency. It does not care if you ‘felt like’ eating greens that day. It does not care if your kale was organic or your spinach was ‘locally sourced.’ It cares about micrograms. It cares about rhythm. It cares about predictability.
And yet, we treat it like a suggestion. Like a wellness trend. Like something we can cherry-pick based on mood.
My cousin, a former yoga instructor, went on a ‘green detox’-three days of kale smoothies. Her INR dropped to 1.1. She developed a pulmonary embolism. She survived. But she lost six months of her life in the hospital.
This isn’t about food. It’s about reverence. Treat your vitamin K intake like your insulin dose. Like your blood pressure meds. Not optional. Not trendy. Essential. Non-negotiable.
Consistency isn’t boring. It’s sacred.
Shubham Mathur
December 16, 2025 AT 18:34Look I’ve been on warfarin for 18 years and I’ve seen every dumb trend out there. People think they’re being smart by eating ‘clean’ but they don’t realize that one giant salad can tank your INR in 48 hours. And no you don’t need to count mcg. Just pick one green and stick with it. I eat 1/2 cup cooked spinach every single day. No more no less. Done. If I go out? I order the same thing. Same portion. Same prep. That’s it. No drama. No guilt. No ‘but I’m healthy’ nonsense. This isn’t about being healthy. It’s about staying alive. Stop making it harder than it is. Consistency. Not restriction. That’s the only rule. And if you can’t do that? Then you shouldn’t be on warfarin. Period.
Iris Carmen
December 18, 2025 AT 13:48honestly i just eat the same frozen spinach every night and call it a day. no measuring. no diary. just one cup. same time. same bowl. my inr’s been stable for 5 years. i dont even think about it anymore. it’s just… part of dinner. like salt. or pepper. weirdly calming tbh.