Zestril (Lisinopril) vs Common Blood Pressure Alternatives: A Practical Comparison
 Oct, 4 2025
Oct, 4 2025
Choosing the right pill for high blood pressure can feel like a guessing game. Zestril (the brand name for lisinopril) is a household name, but dozens of other drugs promise similar control. This guide breaks down how Zestril stacks up against the most common alternatives, so you can decide which one fits your health profile, lifestyle, and budget.
What is Zestril (Lisinopril)?
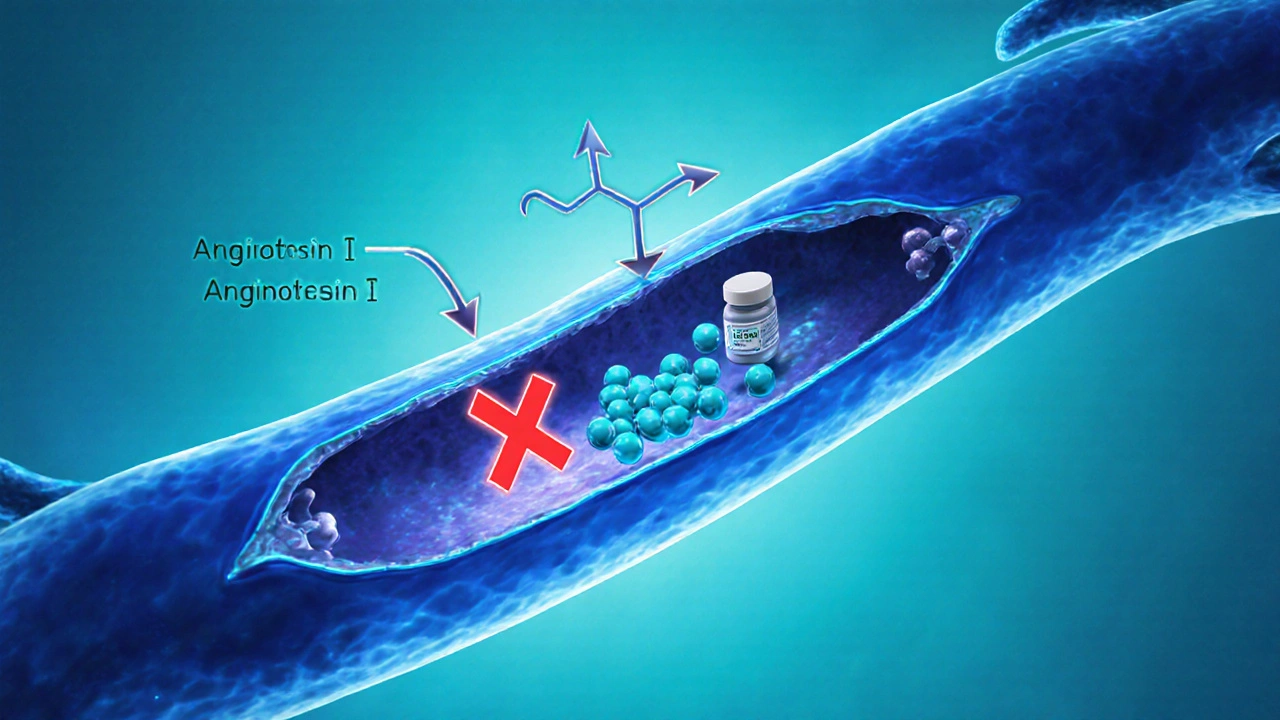
Zestril is the trade name for lisinopril, an ACE (angiotensin‑converting enzyme) inhibitor used to treat hypertension, heart failure, and to improve survival after heart attacks. By blocking the enzyme that narrows blood vessels, it helps vessels stay relaxed, lowering the pressure the heart must pump against.
How Zestril Works and Typical Use
Lisinopril blocks the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor. The result is a drop in systemic vascular resistance and, consequently, lower blood pressure. Most adults start on 10mg once daily; doses can be titrated up to 40mg based on response and tolerability.
Common side effects include a persistent cough, elevated blood potassium, and occasional dizziness. Rare but serious risks are angio‑edema (swelling of lips, tongue, or throat) and kidney function decline. Because it’s excreted through the kidneys, doctors monitor creatinine and electrolytes, especially in patients with pre‑existing kidney disease.
Why Look at Alternatives?
Not everyone tolerates ACE inhibitors well. A dry cough, for example, drives many patients to switch. Some people have contraindications, such as a history of angio‑edema or pregnancy. Cost can also sway decisions-generic lisinopril is cheap, but insurance formularies sometimes favor other agents.
Key Alternatives to Zestril
- Enalapril - another ACE inhibitor with a similar mechanism but a slightly shorter half‑life, often dosed twice daily.
- Losartan - an ARB (angiotensinII receptor blocker) that blocks the same pathway downstream, making it a go‑to for ACE‑intolerant patients.
- Amlodipine - a calcium‑channel blocker that relaxes vascular smooth muscle through a completely different mechanism, useful in patients with isolated systolic hypertension.
All three are widely prescribed, generic, and covered by most health plans in Australia and globally.
Comparison Criteria
To decide which drug suits you, consider these factors:
- Mechanism of action - influences side‑effect profile and drug interactions.
- Blood‑pressure reduction efficacy - measured by average mmHg drop in clinical trials.
- Dosage flexibility - once‑daily vs. multiple doses.
- Side‑effect spectrum - cough, dizziness, electrolyte changes, etc.
- Cost & insurance coverage - retail price per month and typical PBS (Pharmaceutical Benefits Scheme) listing.
- Special population suitability - kidney disease, pregnancy, diabetes, older adults.
Side‑by‑Side Comparison Table
| Drug | Class | Typical Starting Dose | Average BP Drop (mmHg) | Common Side Effects | Special Notes |
|---|---|---|---|---|---|
| Zestril (Lisinopril) | ACE inhibitor | 10mg once daily | ≈12/8 | Cough, hyperkalaemia, dizziness | Avoid in pregnancy; monitor kidney function |
| Enalapril | ACE inhibitor | 5mg once daily (or 2.5mg BID) | ≈10/7 | Cough, rash, renal decline | Shorter half‑life; may need twice‑daily dosing |
| Losartan | ARB | 50mg once daily | ≈11/6 | Dizziness, hyperkalaemia (less cough) | Preferred if ACE‑induced cough is an issue |
| Amlodipine | Calcium‑channel blocker | 5mg once daily | ≈9/5 | Peripheral edema, flushing, headache | Very effective for isolated systolic hypertension; can combine with ACE/ARB |
Best‑Fit Scenarios
- First‑line for most adults: Zestril offers once‑daily dosing, strong evidence, and low cost.
- ACE‑intolerant (cough or angio‑edema): Switch to Losartan or another ARB; they avoid the cough while delivering similar BP drops.
- Kidney disease (stage3‑4): Start low, monitor creatinine. Some clinicians favour Enalapril because its shorter half‑life allows quicker adjustments.
- Isolated systolic hypertension in seniors: Amlodipine’s vasodilatory effect on arterial stiffness can be more beneficial.
- Pregnant patients: ACE inhibitors and ARBs are contraindicated. Alternative classes (e.g., methyldopa) are needed - not covered in this table.
Cost Snapshot (Australian PBS 2025)
All four drugs are listed on the PBS, meaning a standard co‑payment of AU$6.90 per prescription. However, brand‑named Zestril may still appear on some private scripts at around AU$20 for a thirty‑day supply, whereas generic lisinopril, enalapril, losartan, and amlodipine typically sit under AU$10.
Key Takeaways
- Zestril is a proven, once‑daily ACE inhibitor with robust BP‑lowering data.
- Losartan is the go‑to swap if a cough or angio‑edema makes ACE inhibitors unsafe.
- Enalapril offers similar efficacy but often requires twice‑daily dosing.
- Amlodipine works through a different pathway, ideal for older adults with stiff arteries.
- Cost differences are minimal on the PBS, but brand names can be pricier on the private market.
Frequently Asked Questions
Can I take Zestril with other blood‑pressure meds?
Yes. Many patients combine an ACE inhibitor with a diuretic or a calcium‑channel blocker for added control, but always follow your doctor’s dosing schedule to avoid low blood pressure.
How long does it take for Zestril to start lowering my blood pressure?
Most people see a measurable drop within 1‑2 weeks, with the full effect stabilizing around 4‑6 weeks after the initial dose.
Is the cough from Zestril dangerous?
The cough is usually dry and harmless, but it can be bothersome. If it persists, discuss switching to an ARB like Losartan with your clinician.
What should I monitor while on Zestril?
Regular blood‑pressure checks, blood tests for potassium and kidney function, and any signs of swelling in the face or throat.
Can I use Zestril if I have diabetes?
Yes, and ACE inhibitors often provide extra kidney protection for diabetics, making them a preferred first‑line choice.

Next Steps for Patients
1. Review your current BP readings and any side effects you’ve noticed.
2. Schedule a quick chat with your GP or pharmacist. Bring this comparison - it helps focus the conversation on mechanism, dosing, and cost.
3. If you’re switching from Zestril to an ARB, expect a short overlap period (typically 24‑48hours) before the new drug takes full effect.
4. Keep a simple log: date, dose, BP reading, and any new symptoms. This data lets your clinician fine‑tune the regimen.
Whether you stay on Zestril or move to another option, the goal is the same - keep your blood pressure in the target range, avoid complications, and feel good day‑to‑day.


SHASHIKANT YADAV
October 4, 2025 AT 13:08I've been scanning the tables and the numbers line up nicely – Zestril really does shave off about 12/8 mmHg on average, which is solid for a first‑line agent. 😎 The once‑daily dosing is a win for folks who forget meds mid‑day. The cough side‑effect is the usual trade‑off, but most patients tolerate it. Cost‑wise, the PBS keeps it cheap, so budget isn’t a barrier. Overall, it’s a reliable workhorse in the hypertension toolbox.
Ryan Pitt
October 9, 2025 AT 20:11Totally agree! Keeping it simple with a once‑daily pill makes adherence a breeze, and the blood‑pressure drop is just what the doctor ordered.
Jami Johnson
October 15, 2025 AT 03:15When you peel back the layers of hypertension management, the story of ACE inhibitors like Zestril reads like a classic epic of biochemical sabotage. The drug strides onto the stage by halting the conversion of angiotensin I into the notorious vasoconstrictor angiotensin II, a move that relaxes the arterial highway and eases the heart’s workload. This mechanistic elegance translates into a consistent systolic‑diastolic reduction, typically hovering around twelve over eight millimetres of mercury, a figure that has withstood decades of clinical scrutiny. Yet, the narrative does not end with blood‑pressure numbers; ACE inhibitors also bestow renal protection, especially crucial for patients battling diabetes‑induced nephropathy. The protective veil stems from reduced intraglomerular pressure, which slows the march of microalbuminuria. However, the saga is not without its villains – the dry cough, an insidious side‑effect, haunts up to a quarter of users, prompting many to abandon the quest for an ARB like Losartan. Angio‑edema looms as a rarer but more terrifying adversary, capable of turning a routine prescription into a medical emergency. For clinicians, the balancing act involves monitoring serum potassium and creatinine, ensuring that the kidneys remain unscathed. The drug’s elimination via renal pathways means that dose adjustments become paramount in chronic kidney disease, where a gentler initiation may forestall iatrogenic harm. Cost considerations, while often muted by universal schemes, still surface when brand‑name Zestril slips into private prescriptions, inflating the patient’s out‑of‑pocket burden. When juxtaposed with Enalapril, the half‑life difference nudges dosing frequency, nudging some patients toward twice‑daily regimens for tighter control. Losartan, the ARB sibling, sidesteps the cough by targeting the receptor downstream, offering a comparable pressure dip without the pulmonary irritation. Amlodipine, hailing from the calcium‑channel camp, tackles isolated systolic hypertension with a distinct vasodilatory flourish, yet it may provoke peripheral edema. The therapeutic tapestry thus weaves together potency, side‑effect profiles, renal implications, and economic threads, demanding a personalized selection for each patient. In practice, the decision matrix resembles a chessboard, where each move – drug choice, dose, combination – anticipates future clinical scenarios. Ultimately, Zestril’s legacy endures because it delivers dependable pressure control, a safety net for the kidneys, and a cost‑effective profile that keeps the healthcare system humming.
Kasey Krug
October 20, 2025 AT 10:18While thorough, the piece glosses over the real‑world adherence issues that arise when patients experience even a mild cough.
jake cole
October 25, 2025 AT 17:22This so‑called “practical comparison” is nothing but a laundry‑list of generic fluff that anyone with a pharmacy degree could copy‑paste. Stop pretending this is original insight.
Natalie Goldswain
October 30, 2025 AT 23:26lol i get it, zestril is cheap but if u got insurance it's barely a thing. just ask ur doc if the cough is worth it.
khajohnsak Mankit
November 5, 2025 AT 06:29The pharmacologic ballet of lisinopril pirouettes across the angiotensin axis, painting vascular serenades that whisper tranquility into the hyper‑tense arteries.
Jayant Paliwal
November 10, 2025 AT 13:33Consider, if you will, the spectrum of therapeutic options; each drug-whether ACE inhibitor, ARB, or calcium‑channel blocker-offers a unique constellation of effects, benefits, and drawbacks. The clinician, armed with this data, must navigate an intricate maze of patient histories, comorbidities, and socioeconomic factors, all while balancing efficacy against tolerability. Zestril, for instance, provides a robust reduction in systolic pressure, yet its propensity to induce a dry cough cannot be ignored; this side‑effect, while benign for many, can precipitate non‑adherence. Enalapril, sharing a similar mechanism, demands more frequent dosing, which may introduce its own set of challenges. Losartan sidesteps the cough, offering comparable efficacy, but may be pricier in certain markets. Amlodipine, operating through calcium channel modulation, excels in isolated systolic hypertension, though it may cause peripheral edema. The decision‑making process, therefore, resembles a complex equation where variables such as renal function, pregnancy status, and concomitant medications must be meticulously accounted for. In the end, no single agent reigns supreme; the optimal regimen emerges from a personalized synthesis of evidence, patient preference, and clinical judgment.
Kamal ALGhafri
November 15, 2025 AT 20:36In the grand theater of cardiovascular regulation, each molecule assumes a role scripted by evolutionary necessity, urging us to contemplate whether prescribing is an act of dominion or partnership.
Gulam Ahmed Khan
November 21, 2025 AT 03:40Great point! Keeping the conversation focused on individual patient needs makes the comparison so much more useful 😊
John and Maria Cristina Varano
November 26, 2025 AT 10:43This article is a total waste of time.
Melissa Trebouhansingh
December 1, 2025 AT 17:47One cannot help but observe that the author, in an attempt to distill the complexities of antihypertensive pharmacotherapy, has inadvertently reduced a nuanced clinical discourse to a series of tabular entries that, while ostensibly informative, betray a certain myopia regarding patient‑centred care. The reductionist approach, privileging numerical averages over the lived experience of cough, edema, and the psychosocial ramifications of chronic medication, risks rendering the treatise an exercise in academic minimalism rather than a pragmatic guide. Moreover, the omission of discourse on drug‑drug interactions-particularly the perilous synergy between ACE inhibitors and potassium‑sparing diuretics-leaves a lacuna that discerning clinicians should rightfully lament. While the cost analysis, anchored to Australian PBS figures, provides a useful benchmark, it fails to interrogate the broader economic implications of polypharmacy and the downstream costs of adverse events. In sum, the composition, though competent in its factual conveyance, would benefit from an infusion of narrative depth that acknowledges the heterogeneity of patient narratives beyond the sterile confines of a spreadsheet.
Brian Rice
December 7, 2025 AT 00:50Upon rigorous examination, the presented data reveal a conspicuous absence of randomized control trial citations, thereby undermining the purported evidentiary foundation of the comparison.
Stan Oud
December 12, 2025 AT 07:54Sure, the table is neat… but real patients don’t care about mmHg figures; they care about feeling better – which this piece conveniently ignores.
Ryan Moodley
December 17, 2025 AT 14:57It is nothing short of intellectual laziness to parade a side‑by‑side table as if it were a revelation; the true art of medicine lies in nuanced judgment, not in sterile grids.
carol messum
December 22, 2025 AT 22:01Reflecting on the mechanisms, it becomes clear that the choice between ACE inhibitors and ARBs often hinges on patient tolerance rather than sheer efficacy.
Jennifer Ramos
December 28, 2025 AT 05:04Thanks for the thorough breakdown! I think adding a quick checklist for clinicians could make applying this info even easier 😊
Grover Walters
January 2, 2026 AT 12:08In conclusion, while Zestril remains a cornerstone of antihypertensive therapy, the decision to switch to an alternative must be guided by individualized risk‑benefit assessment, comorbid conditions, and patient preference.